Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Antiphospholipid antibodies (aPL) have been associated with organ damage and certain features in SLE patients. Our aim is to investigate the association between the different aPL and SLE manifestations as well as to elucidate the influence of the load of antibodies.
Methods: Patients from the RELESSER-T registry were included. RELESSER-T is a multicenter, hospital-based registry, with retrospective cross-sectional collection of data from a large representative sample of adult non-selected patients with SLE attending Spanish rheumatology services from the public national health system.
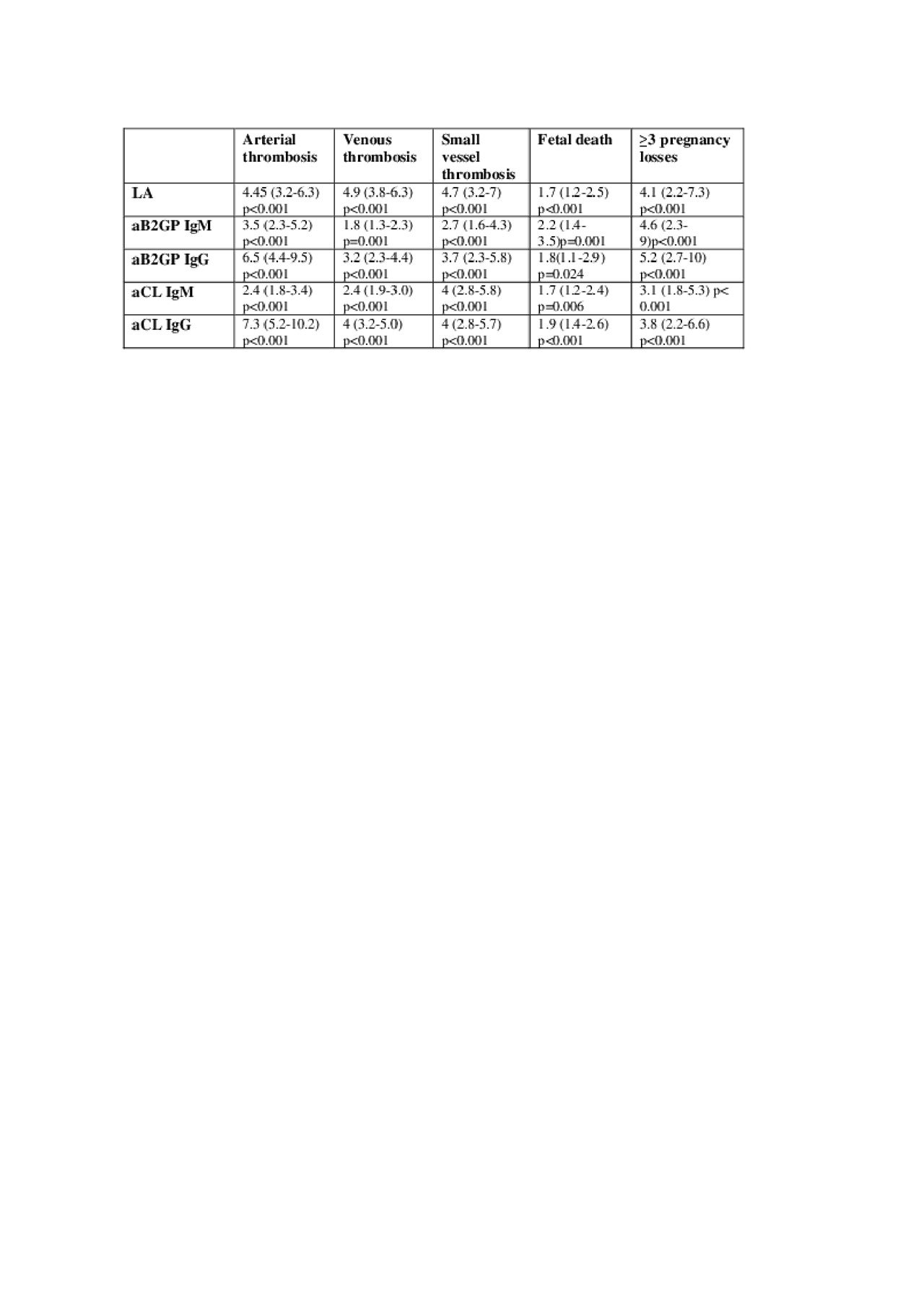
Results: Out of a total of 3651 SLE patients, 1368 were aPL positive (24.8 % were positive for IgG anticardiolipin (aCL) antibodies, 20.1% for IgM aCL, 13.5% showed positivity for IgG antib2glycoprotein I (aB2GPI) and 13.8% for IgM aB2GPI. Lupus anticoagulant (LA) was positive in 24% of patients). Regarding the load of antibodies, 20.6%, 12.1% and 4.8% were positive for one, two and three antibodies respectively. The association between the different aPL, the number of positive antibodies and antiphospholipid syndrome related manifestations is showed in Table 1. Overall, all types of aPL were associated with classic APS manifestations, although LA, IgG isotypes, and patients with more than one aPL display a higher risk to develop clinical APS. Regarding specific lupus manifestations, all aPL types showed a negative association with cutaneous manifestations. LA and aCL were associated with an increased risk of haematological, ophthalmological and neuropsychiatric manifestations (p< 0.001). Furthermore, LA was also associated with an increased risk of renal disease (p< 0.001). IgG isotypes were associated with a higher risk of specific lupus manifestations compared with IgM. IgG aCL were associated with an increased risk of cardiac and respiratory manifestations. When evaluating the influence of the load of antibodies, we found that the risk of neuropsychiatric manifestations significantly increased with a higher number of positive antibodies (OR for one antibody was 1.19 and 1.7 for 2 and 3 antibodies). Inversely, the risk of cutaneous symptoms decreased while the number of positive antibodies increased (OR=0.9 for one antibody, OR=0.8 for double positivity and OR=0.7 for triple positivity).
Conclusion: There is a hierarchy for aPL and the risk of APS and SLE manifestations. aCL, and especially LA, confer a higher risk for major organ involvement in SLE patients. IgG isotypes seem to have a more important role. The load of aPL confer a higher risk for APS and certain SLE manifestations
To cite this abstract in AMA style:
Riancho-Zarrabeitia L, Martinez-Taboada V, Rua Figueroa I, Alonso F, Galindo M, Ovalles-Bonilla J, Olivé-Marqués A, Fernández-Nebro A, Calvo-Alen J, Menor Almagro R, Tomero-Muriel E, Uriarte Isacelaya E, Boteanu A, Andrés M, Freire González M, Santos Soler G, Ruiz Lucea E, Ibañez Barcelo M, Castellvi I, Galisteo C, Quevedo Vila V, Raya E, Narváez J, Expósito L, Hernández-Beriain J, Horcada Rubio L, Aurrecoechea E, Pego-Reigosa J. Do All Antiphospholipid Antibodies Confer the Same Risk for Major Organ Involvement in Systemic Lupus Erythematosus Patients? [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/do-all-antiphospholipid-antibodies-confer-the-same-risk-for-major-organ-involvement-in-systemic-lupus-erythematosus-patients/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/do-all-antiphospholipid-antibodies-confer-the-same-risk-for-major-organ-involvement-in-systemic-lupus-erythematosus-patients/