Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is a systemic autoimmune disease with the potential to severely diminish patients’ quality of life (QoL). SLE disproportionately affects young Black females in both prevalence and disease severity. One goal of this study was to measure the impact of race and other demographic features on mental and physical QoL domains in patients with SLE compared to controls.
Methods: This study was nested in a longitudinal IRB-approved observational registry of patients with SLE and population-matched unaffected controls. We included adults ≥18 years with and without diagnosed SLE who completed at least one 36-Item Short Form version 2 (SF-36) questionnaire. The SF-36 includes 4 physical component score (PCS) domains and 4 mental component score (MCS) domains. Disease damage was measured using the SLICC/ACR Damage Index (SDI). Comparisons were made between demographic factors, disease factors, and SF-36 scores using t-tests for continuous variables, Chi-squared tests for categorical variables, and multivariable logistic regression.
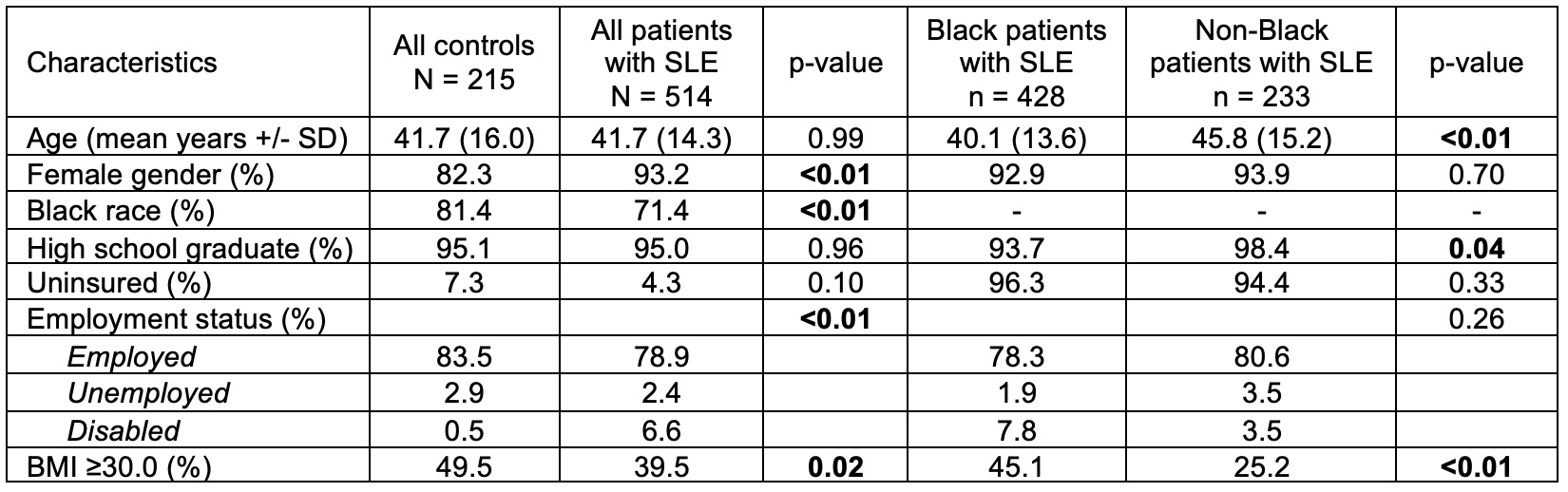
Results: Included were 514 patients with SLE (71.4% identified as Black, 93.2% female) and 215 controls (81.4% Black, 82.3% female). There were no statistically significant differences between patients and controls in high school graduation or insurance status (comparing insured to uninsured), however a greater proportion of controls had private insurance (76.1% vs. 57.3%, p< 0.01). (Table 1)
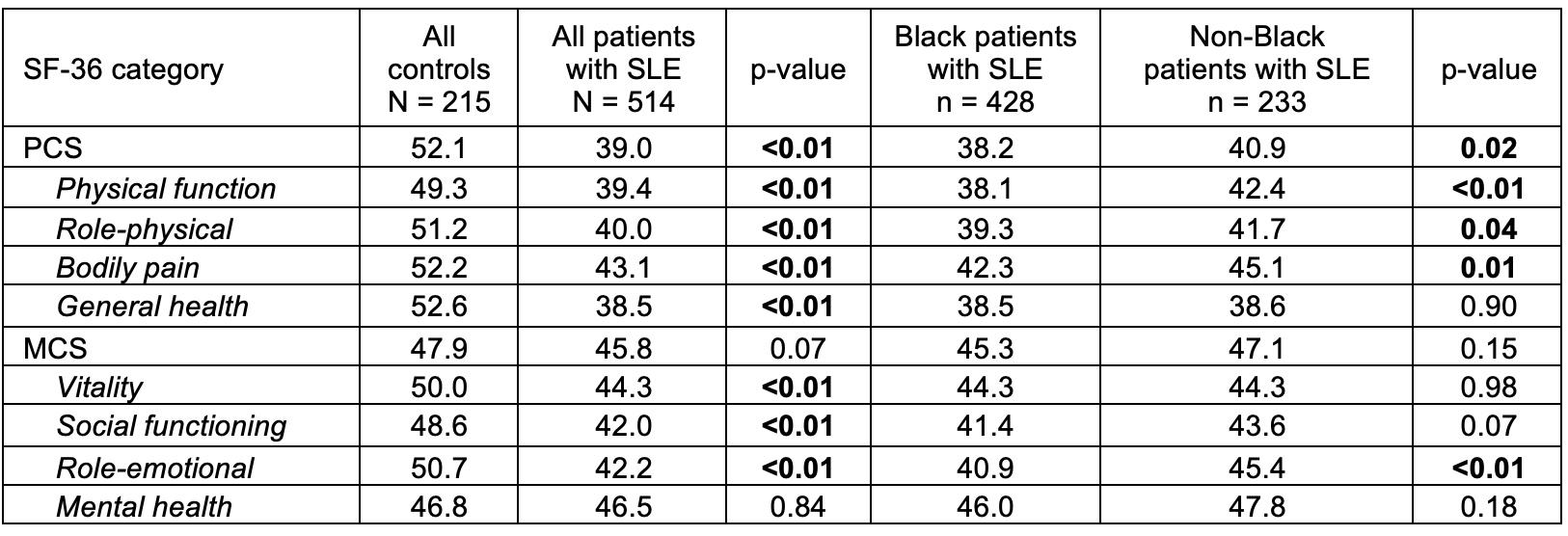
When comparing QoL scores, patients with SLE had significantly worse scores in all domains compared to controls (all p< 0.01) except mental health (p=0.84). Compared to non-Black patients with SLE, Black patients had significantly worse SF-36 scores in 3 of the 4 PSC domains (physical function, role-physical, bodily pain) and 1 of the 4 MSC domains (role emotional). Although the total PCS was worse in Black patients (38.2±11.2 vs 40.9±12.9, p=0.02), the total MCS was similar between Black and non-Black patients (p=NS). (Table 2)
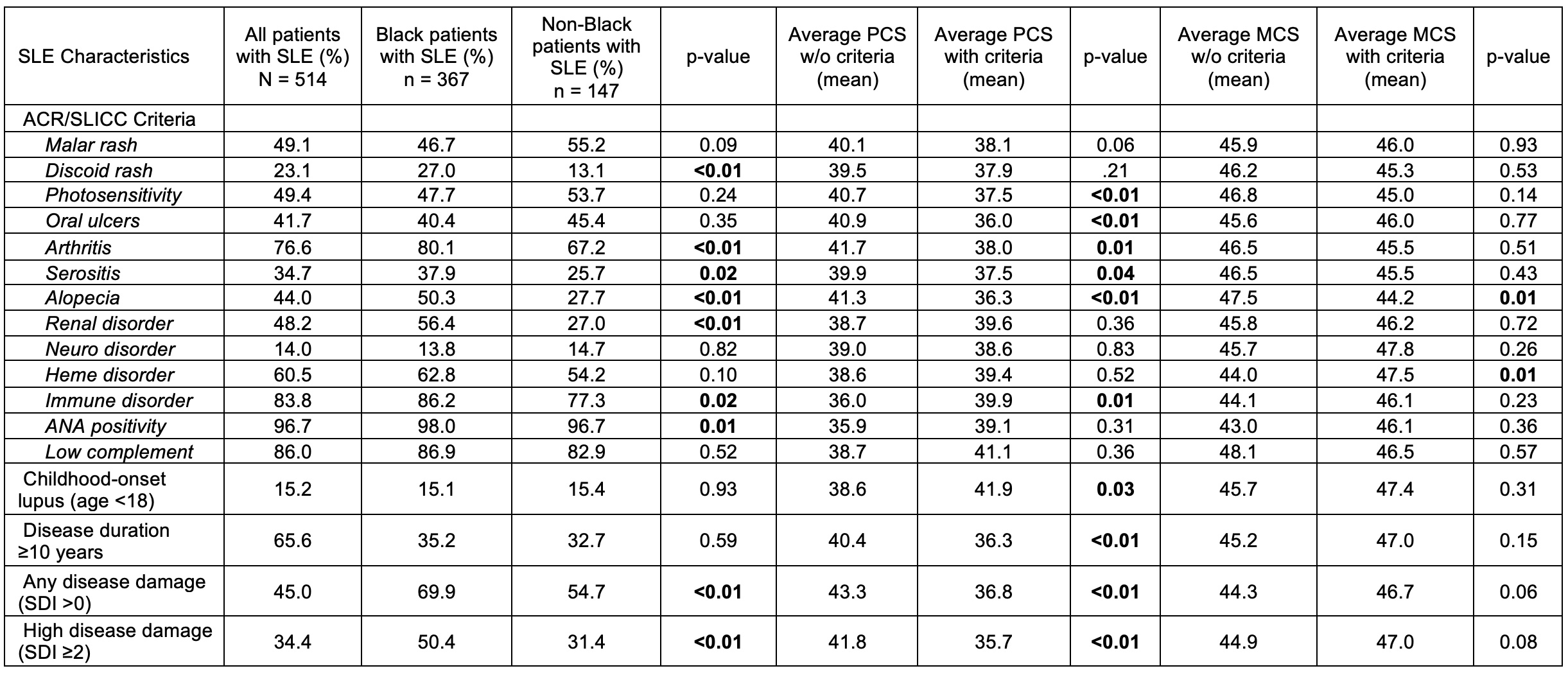
Black patients with SLE compared to non-Black had higher rates of discoid rash (21.0 vs 13.1, p< 0.01), alopecia (50.3% vs. 27,7%, p< 0.01), arthritis (80.1% vs. 67.2%, p< 0.01), renal disease (56.4% vs. 27.0, p< 0.01), any disease damage (SDI >0) (69.9% vs. 54.7%, p< 0.01), and high disease damage (SDI≥2) (50.4% vs. 31.4%, p< 0.01). MCS and PCS scores were not significantly different in patients with compared to without renal disease. Over 68.8±44.6 months of follow-up, patients with SLE had no significant change in PCS scores but had a significant improvement in MSC scores over time (by 1.6±11.4, p=0.02), predominately among the Black patients (by 1.8±11.9, p=0.02). In a multivariate regression model, there was no significant association between Black race and either total PCS or MCS once adjusted for age, disease duration, sex, insurance status, BMI, SDI damage score, and depression. (Table 3)
Conclusion: In addition to previously reported disparities in health outcomes between Black and non-Black patients with SLE, our study finds substantial differences in self-reported QoL that are likely multifactorial in etiology. The continuation of this work will help inform future interventions to improve QoL for patients with SLE.
To cite this abstract in AMA style:
Delk V, Wilson D, Gilkeson G, Oates J, Kamen D. Disparities in Health-Related Quality of Life Among Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/disparities-in-health-related-quality-of-life-among-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/disparities-in-health-related-quality-of-life-among-patients-with-systemic-lupus-erythematosus/