Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Evidence on the treatment of enthesitis, a common feature of psoriatic arthritis (PsA), is limited. This post-hoc, cross-sectional study examined if prevalent treatment choices were related to enthesitis, or other prevalent characteristics of PsA patients.
Methods: Patients enrolled in the Corrona PsA database were included in this study if they had prevalent use of therapeutic drugs and indication of clinical enthesitis. Prevalent use was defined as drug initiation at least two months prior to visit. Enthesitis was defined as having at least one tender point of the 18 sites described by the validated enthesitis scoring index, spondyloarthritis research consortium of Canada (SPARCC) enthesitis index. Treatments groups included cDMARDs, TNF inhibitors (TNFi), and IL-17 inhibitors (IL-17i). The primary outcome was the association of enthesitis activity across different therapies. Secondary outcomes included differences between drug groups in the following disease domain measurements: CDAI, psoriasis body surface area (BSA) %, 68 tender joint count, 66 swollen joint count, health assessment questionnaire (HAQ) score, patient reported pain, patient reported fatigue score, patient global assessment, physician global assessment, and work productivity and activity impairment (WPAI) questionnaire. One-way analysis of variance was used to determine the association between SPARCC scores and prevalent drug use after adjusting for covariates at baseline. Logistic regression (unadjusted analysis) was used to find an association between disease activity and prevalent drug use. Principal component analysis (PCA) derived the primary dimensions of disease activity scores and examined for patterns of clustering among the different prevalent drug groups based on such scores.
Results: 394 PsA patients with enthesitis were identified with 151 patients taking a cDMARD, 167 patients taking a TNFi and 76 patients taking a IL-17i. Complete patient demographics are presented in Table 1. There was a trend of lower SPARCC scores in the IL-17i (3.09+2.54) and TNFi groups (3.28+2.62) as compared to the cDMARD group (3.87+3.28) but the global p-score was not statistically significant. Complete analysis of other disease domain scores is presented in Table 2. With age and disease duration excluded, lower physician global assessment and lower mHAQ scores were associated with prevalent TNFi use when compared to cDMARD use (Table 2). Lower physician global assessment was associated with prevalent IL-17i use compared to cDMARD use. Age, duration of disease course, nor any disease activity measures were associated with prevalent use of TNFi compared to IL-17i. PCA resulted in three major dimensions representing 72% of the variation. Plots of the scores illustrated similar distributions of scores among the drug groups that mainly overlapped with no particular clustering (Figure 1).
Conclusion: Prevalent drug utilization was not related to enthesitis activity. Patients with prevalent use of cDMARDs were noted to have higher physician global assessment scores compared to TNFi and IL-17i use. In aggregate, there was no pattern of correlation in disease activity scores amongst the use of different prevalent PsA drug therapies.
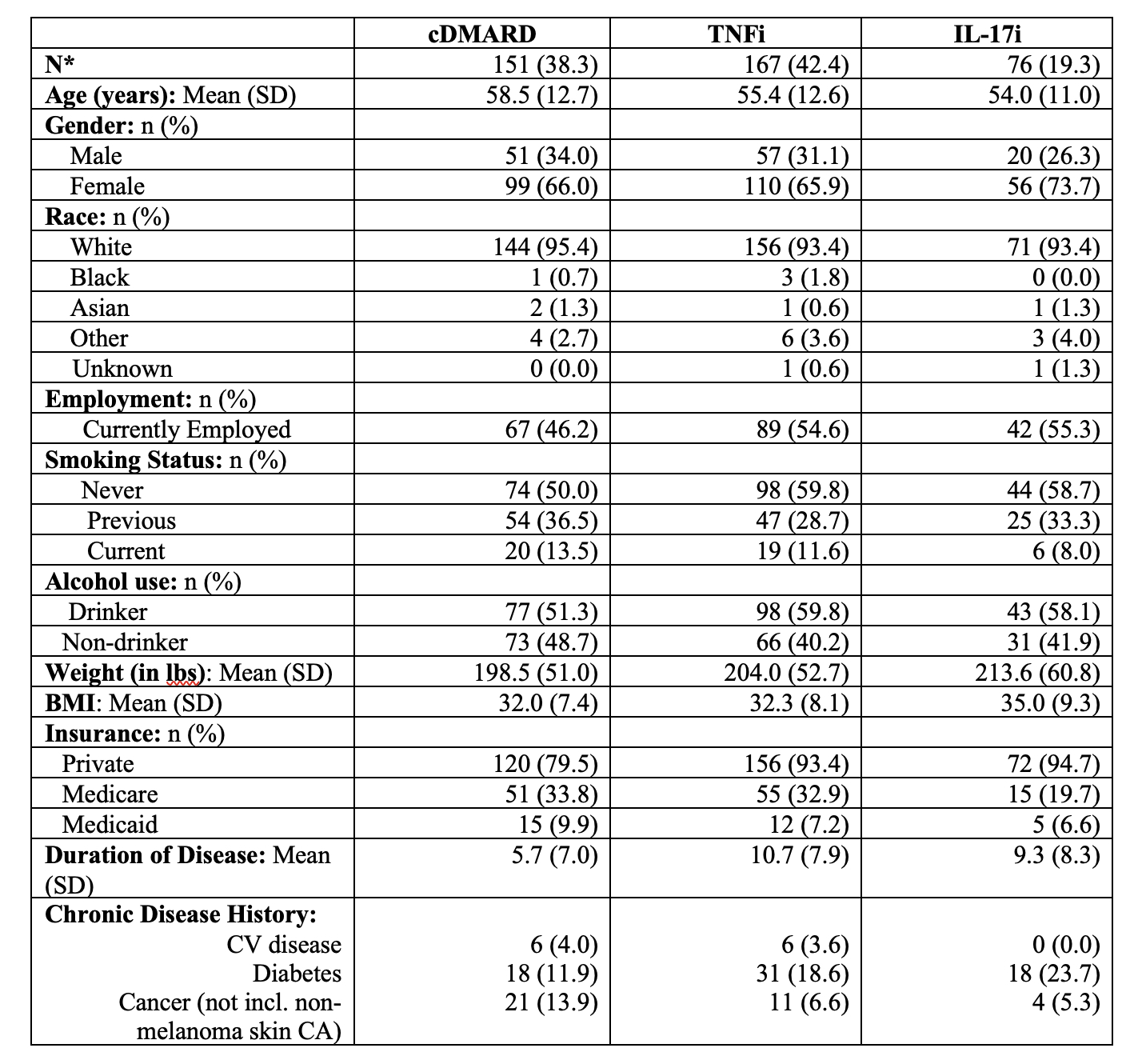 Table 1: Patient Characteristics
Table 1: Patient Characteristics
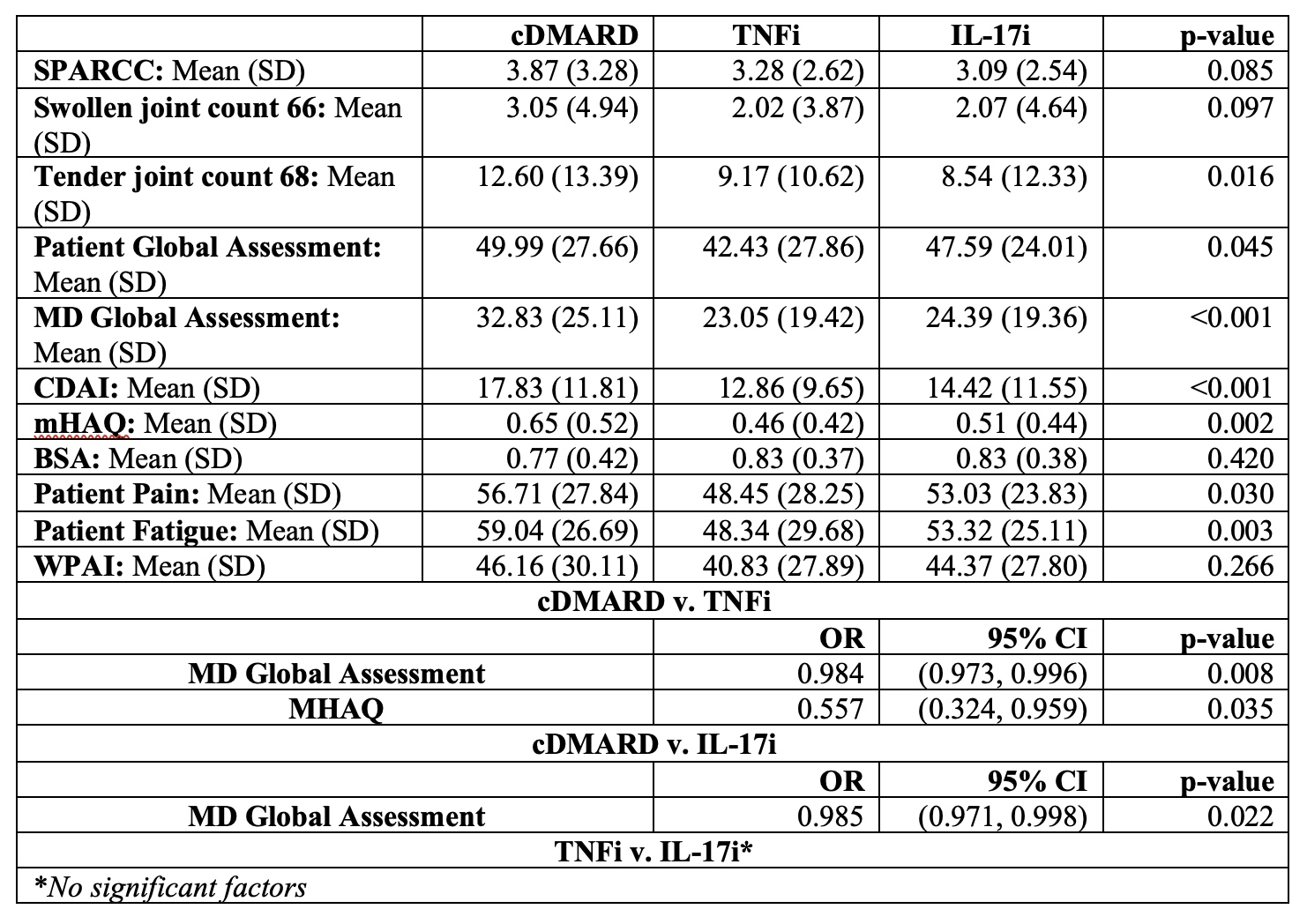 Table 2: Comparison of disease activity measures by drug and Logistic Regression Model Across Different Drugs
Table 2: Comparison of disease activity measures by drug and Logistic Regression Model Across Different Drugs
 Figure 1: Principle component analysis of PsA disease activity measures across different therapies
Figure 1: Principle component analysis of PsA disease activity measures across different therapies
To cite this abstract in AMA style:
Chao R, Reed G, Kremer J, Kavanaugh A. Disease Activity in Psoriatic Arthritis Patients with Enthesitis Across Different Therapies [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/disease-activity-in-psoriatic-arthritis-patients-with-enthesitis-across-different-therapies/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/disease-activity-in-psoriatic-arthritis-patients-with-enthesitis-across-different-therapies/
