Session Information
Date: Saturday, November 12, 2022
Title: Vasculitis – Non-ANCA-Associated and Related Disorders Poster I: Giant Cell Arteritis
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: A prior study evaluated incidence rates of biopsy proven giant cell arteritis (GCA) among black and white patients, concluding that GCA occurs at a similar rate in both groups. Our hypothesis, based on clinical experience at our institution, is that GCA is rare among black patients. To evaluate this, we compared the temporal artery biopsy (TAB) positivity rates among our white and black patients.
Methods: We conducted a retrospective chart review from all patients who underwent TAB at our affiliated Eye Hospital from 2012 until 2021. Data extracted included age, sex, race/ethnicity, presence of non-visual symptoms (headache, jaw claudication, facial pain, or constitutional symptoms), visual symptoms (blurred or complete vision loss – bilateral or monocular, history of transient vision loss), and laboratory data (sedimentation rate, C-Reactive Protein). The main study outcome was the rate of positivity in the TAB. Patients with biopsies that were non-diagnostic, but had an abnormal internal elastic lamina were considered negative. Sensitivity analysis were also done considering this group as positive. The main independent variable for our study was race/ethnicity: patients were grouped as general population (all patients), white, and black patients per administrative demographics in the electronic medical record.Clinical and demographic features of patients undergoing TAB were compared between those with positive and negative biopsies with t tests, Wilcoxon rank sum test, Chi-squared test, or Fisher’s exact test where appropriate. A logistic regression was performed with factors found to be significant at p< 0.1 in bivariate analysis to evaluate for independent associations with a positive biopsy, with special attention to race/ethnicity. However, jaw claudication and constitutional symptoms could not be included in logistic regression due to amount of missing data. A p value of < 0.05 was considered statistically significant in this analysis.
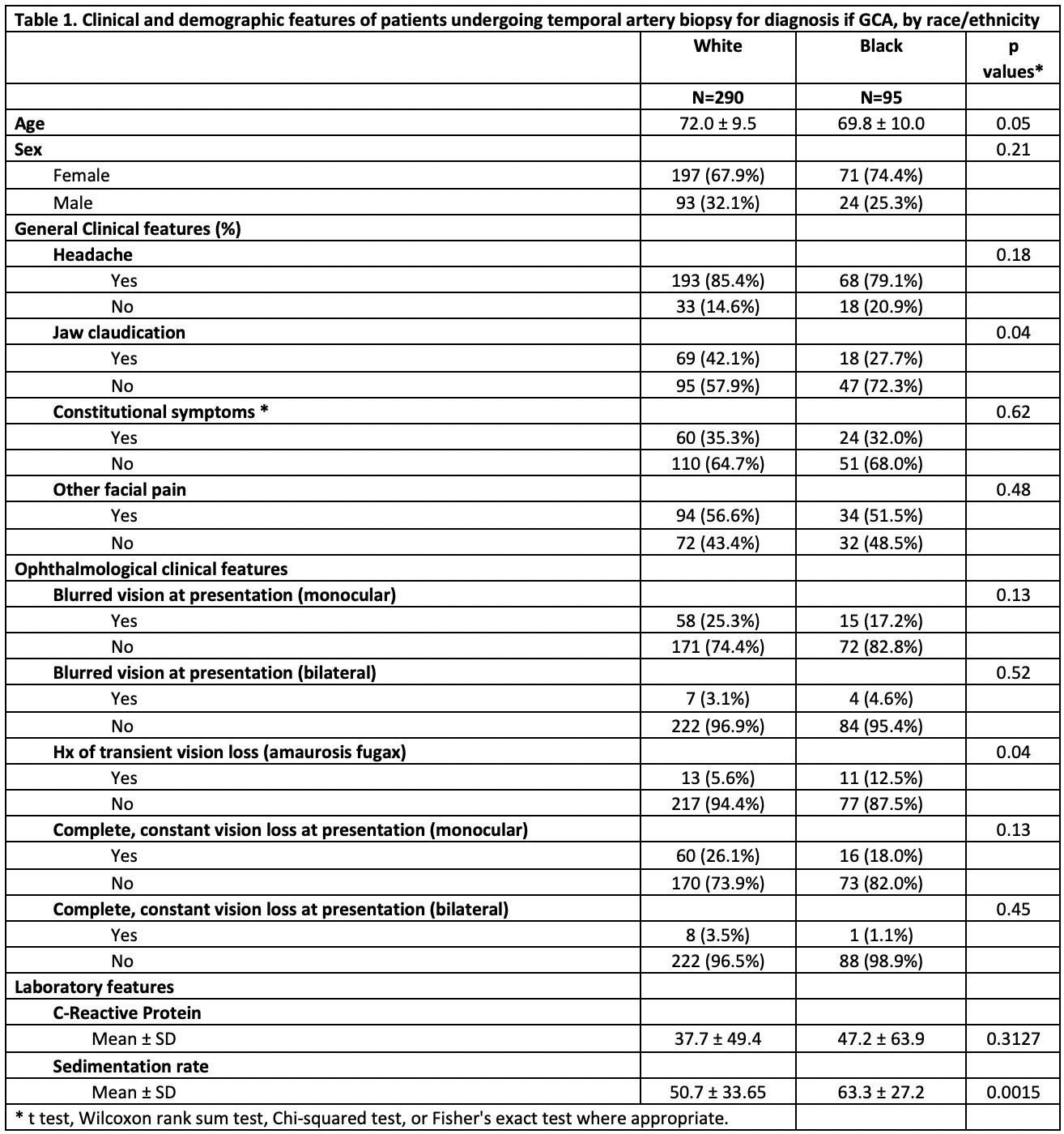
Results: Data from 385 patients who had TAB performed for suspected GCA were included (290 white, 95 black). White and black patients had similar demographic and clinical characteristics, otherwise the only difference was higher mean ESR in black patients (Table 1).
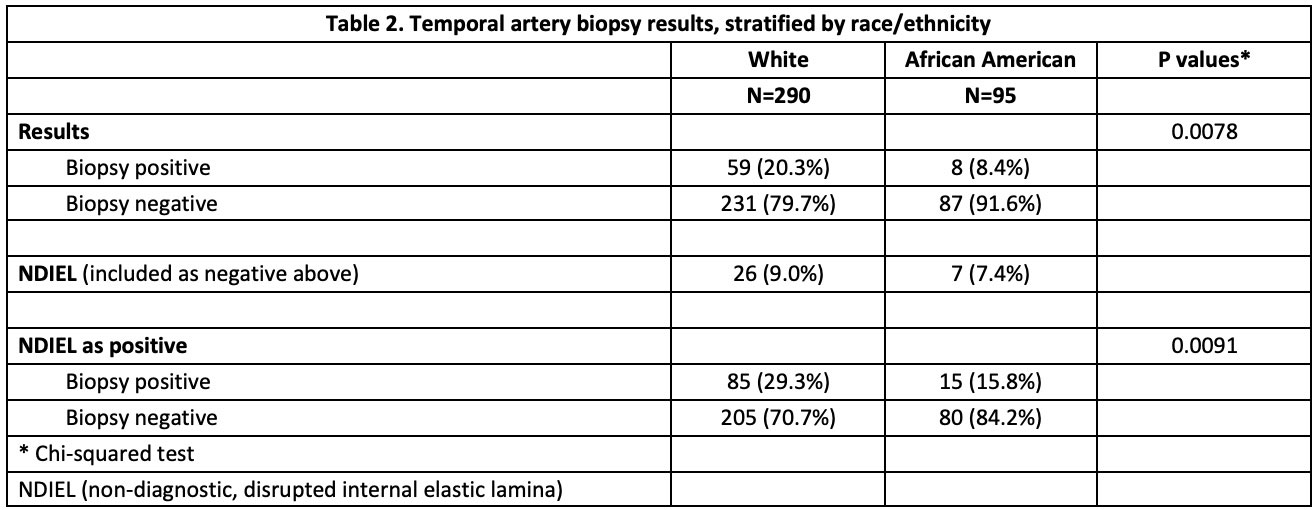
Of all patients referred for TAB, 17.4% (65 patients) had a result diagnostic for GCA. Positivity rate in white patients was 20.3% and 8.4% in black patients (Table 2). 33 biopsies (8.6%) were non-diagnostic with only internal elastic lamina disruption (Table 2). Patients with positive TAB were more likely to have jaw claudication, constitutional symptoms and higher inflammatory markers (Table 2). In the logistic regression analysis for factors independently associated with a positive result in TAB, white race compared to black race was associated with a significant odds ratio of 3.47 (95%CI:1.14-10.59, p < 0.03). Another factor associated with a positive biopsy was age, and there was a negative association with blurry vision (Table 3). Sensitivity analysis did not change our results.
Conclusion: Our study supports the hypothesis that there is a discrepancy in the frequency of GCA, in this case through the positivity rate in TAB, between black patients and white patients – with lower rates in the former.
To cite this abstract in AMA style:
Vachhani R, Li P, Tavakoli M, Kline L, Gaffo A. Discrepancies in Temporal Artery Biopsy Positivity Rate Among White and Black Patients Suspected of Having Giant Cell Arteritis: Experience from a Tertiary Academic Medical Center [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/discrepancies-in-temporal-artery-biopsy-positivity-rate-among-white-and-black-patients-suspected-of-having-giant-cell-arteritis-experience-from-a-tertiary-academic-medical-center/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/discrepancies-in-temporal-artery-biopsy-positivity-rate-among-white-and-black-patients-suspected-of-having-giant-cell-arteritis-experience-from-a-tertiary-academic-medical-center/