Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The rate of medical disability among patient with systemic lupus erythematosus (SLE) ranges from 20-40% and is associated with a number of socioeconomic, disease-related and clinical factors. Our group has developed a conceptual model of SLE symptoms reflecting the patients’ experience: Type 1 SLE activity includes classic inflammatory manifestations of SLE such as arthritis and serositis, whereas Type 2 SLE activity includes fatigue, depression, widespread pain, sleep dysfunction and perceived cognitive dysfunction. We examined the socioeconomic status of patients within these SLE subtypes and factors associated with disability.
Methods: This was a cross-sectional study of SLE patients (SLICC classification criteria) at a university lupus clinic (September 2018 to March 2019). All patients completed Patient Health Quesionnaire-9 (PHQ-9), 2016 ACR fibromyalgia criteria and socioeconomic surveys. Patients were divided into 4 groups: active Type 1 SLE (SLEDAI ≥ 6, clinical SLEDAI ≥ 4, active lupus nephritis, or PGA ≥ 1.5); active Type 2 SLE (fibromyalgia severity score (FSS) ≥ 10); Mixed SLE (both Type 1 and 2); Minimal SLE (neither Type 1 nor 2). Differences were analyzed by Fisher’s exact test. A step-wise regression analysis examined predictors for disability.
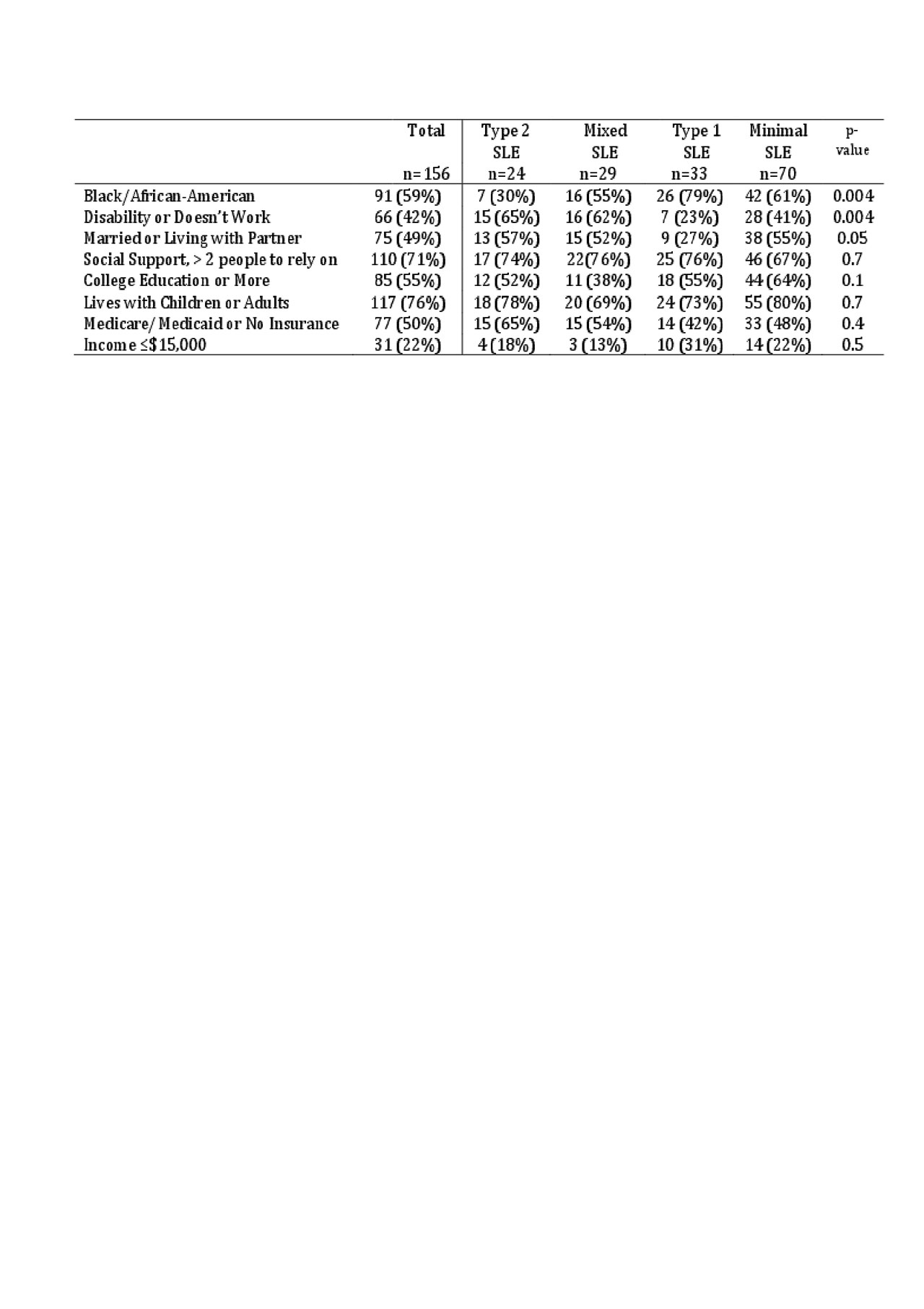
Results: 164 patients completed the surveys (93% female, mean age 43.5 years, 58% Black, 39% Caucasian, 2% Asian, average length of disease 15 years). The demographics of the SLE subtypes were similar, except that more patients with active Type 1 SLE were Black and more with active Type 2 SLE were unable to work (Table 1).
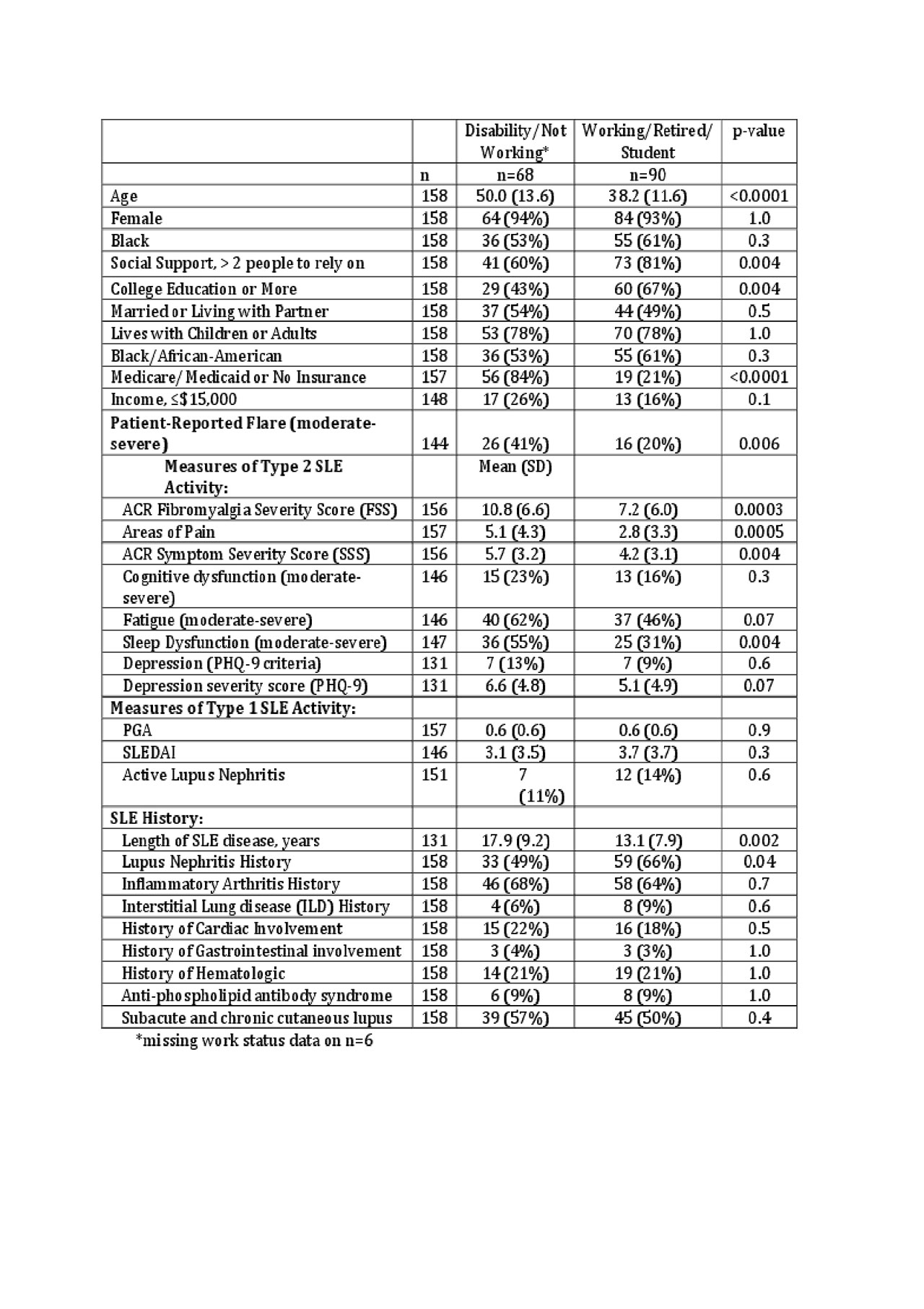
Disabled patients were older, less educated, had less social support, longer disease duration, less historical nephritis, and were more likely to be uninsured or be on Medicare/Medicaid insurance. Furthermore, disabled patients had greater Type 2 symptoms including a higher fibromyalgia severity score (FSS) (10.8 vs 7.2, p = 0.0007), symptom severity score (5.7 vs 4.2, p = 0.005) , more frequent sleep dysfunction (55% vs 31%, p =0.005), and more areas of pain (5.1 vs 2.8, p = 0.005).
There were no differences in current Type 1 SLE activity between patients with and without disability; these two groups had similar SLEDAI and physician’s global assessment, as well as similar features of arthritis, cardiopulmonary, hematologic, or cutaneous SLE.
In multivariate analysis, patients on disability were older (OR 1.07 for every 1 year in age, 95% CI:1.03, 1.12), less educated (OR 2.72, 95% CI: 1.15, 6.45), had a lower income (OR 3.78, 95% CI 1.26, 11.40), and had a higher FSS (OR 1.08 for every 1 point in FSS, 95% CI: 1.00, 1.16).
Conclusion: The overall rate of disability mirrors that of other SLE cohorts, but this study provides evidence that Type 2 not Type 1 SLE that drives SLE patients’ limitations in the workforce. As such, this study suggest that addressing pain, fatigue, and sleep dysfunction could improve health-related quality of life and the care of SLE patients. Incorporating the Type 1 and Type 2 categorization system into clinical practices encourages the provider to focus on all aspects of SLE, including the Type 2 symptoms, which contribute significantly to the high societal cost of SLE.
To cite this abstract in AMA style:
Rogers J, Whitney R, Clowse M, Criscione-Schreiber L, Doss J, Pisetsky D, Sadun R, Sun K, Eudy A. Disability Among Subtypes of SLE [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/disability-among-subtypes-of-sle/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/disability-among-subtypes-of-sle/