Session Information
Date: Tuesday, November 10, 2015
Title: Systemic Lupus Erythematosus - Clinical Aspects and Treatment Poster Session III
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: While diffuse alveolar hemorrhage
(DAH) is recognized as a life-threatening complication of SLE, little is known
about its risk factors and response to therapy. Here, we describe 22 cases of
DAH in a U.S. lupus cohort of ~1,000 patients, and compare them to 66 controls
from the same outpatient cohort.
Methods: All patients met ACR classification
criteria for SLE. We first captured variables pertaining to diagnoses of SLE
and secondary antiphospholipid syndrome (APS) and analyzed them by Chi square (univariate)
testing. Those variables with p values <0.05 were then further considered
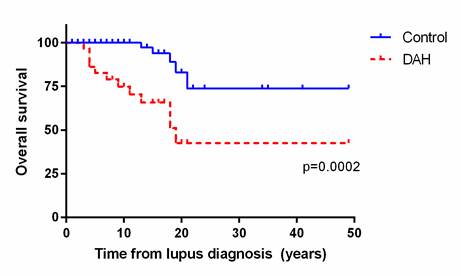
in a multivariate model. Kaplan-Meier curves were constructed for each group,
and survival was analyzed by Log-rank test.
Results: Of the 22 DAH patients, 59% were
diagnosed with DAH within 5 years of SLE diagnosis. By univariate analysis,
several manifestations of SLE and APS were more common in DAH patients as
compared to controls (Table). After building a multivariate model, history
of thrombocytopenia and low C3 were maintained as independent risk factors.
While a remarkable 19/22 DAH patients had a history of thrombocytopenia, only 5
had thrombocytopenia at the time of the DAH episode (and only 2 with platelet
counts <50,000/µl), arguing that DAH was not simply a hemorrhagic
complication of the low platelets. Interestingly, all patients survived their
initial episode of DAH. All were treated with increased immunosuppression,
including various combinations of corticosteroids, plasmapheresis,
cyclophosphamide, rituximab, and mycophenolate mofetil. While the DAH patients
did well in the short-term, their long-term survival was significantly worse compared
to the control group (Figure). Interestingly, despite the history of
both thrombocytopenia and DAH, several of the deaths were attributable to
thrombotic complications after recovering from the DAH episode.
Conclusion:
To our knowledge,
this is the largest case-control study of lupus DAH reported to date. While a history
of thrombocytopenia was strongly predictive of DAH (odds ratio ~40), only 2
patients had platelet counts <50,000/µl at the time of hemorrhage. A number
of APS manifestations correlated with DAH in univariate testing (but not a
multivariate model), and deserve further consideration in larger studies. In
the short-term, this cohort of patients was treated aggressively for their DAH
and fared quite well. However, over time, their survival was significantly reduced
as compared to controls.
To cite this abstract in AMA style:
Kazzaz NM, Coit PS, Lewis EE, McCune WJ, Sawalha AH, Knight JS. Diffuse Alveolar Hemorrhage in SLE: Risk Factors, Response to Therapy, and Survival [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/diffuse-alveolar-hemorrhage-in-sle-risk-factors-response-to-therapy-and-survival/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/diffuse-alveolar-hemorrhage-in-sle-risk-factors-response-to-therapy-and-survival/