Session Information
Date: Saturday, November 6, 2021
Title: Epidemiology & Public Health Poster I: COVID-19 & Vaccination (0084–0117)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Due to the impressive efforts of the global scientific rheumatology community, increasing evidence about inflammatory rheumatic and musculoskeletal diseases (RMD) specific risk factors in the pandemic has been achieved. In this analysis from the German COVID19-Rheuma registry, we analysed the risk factors for the outcome of SARS-CoV-2 infection in patients with RMD, specifically focusing on the impact of the RMD treatment.
Methods: Data from the German physician-reported COVID-19 registry for RMD from March 30th, 2020 until April 9th, 2021 were analysed. Ordinal outcome of SARS-CoV-2 infection severity was defined in three groups: neither hospitalized, ventilated nor deceased; hospitalized with or without non-invasive ventilation, but neither invasively ventilated nor deceased; invasively ventilated or deceased. Independent associations between demographic and disease features and SARS-CoV-2 infection-related severity were estimated by multivariable ordinal logistic regression using the proportional odds model and reported as odds ratio (OR) and 95% confidence interval (CI).
Results: 2,274 patients were included. Baseline characteristics are shown in table 1. 83 patients died, resulting in a case fatality rate of 3.6%.
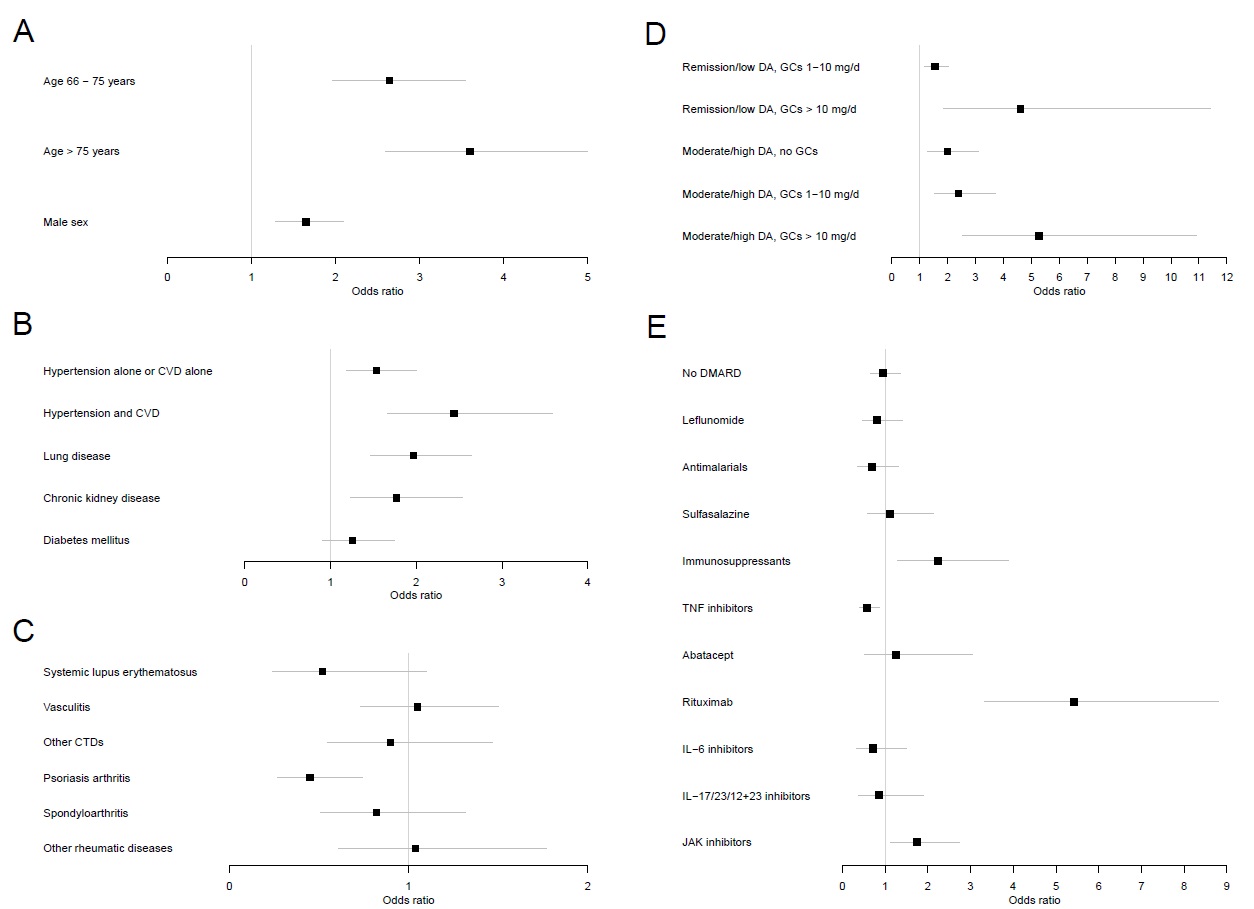
In the ordinal regression analysis, age, male sex, cardiovascular disease, hypertension, chronic lung diseases, and chronic kidney disease were independently associated with a worse outcome of SARS-CoV-2 infection (fig. 1 a, b). Compared to RA, patients with PsA showed a lower OR (fig. 1c). Disease activity and glucocorticoids (GC) were associated with severity of SARS-CoV-2 infection as shown in figure 1d.
For the analysis of the impact of RMD treatment, MTX monotherapy was used as reference. TNFi showed a significant association with a better outcome of SARS-CoV-2 infection. In contrast, immunosuppressants (mycophenolate mofetil, azathioprine, cyclophosphamid, ciclosporin), JAKis and rituximab were independently associated with a worse outcome of SARS-CoV-2 infection (figure 1e).
Conclusion: Known general risk factors for severity of SARS-CoV-2 infection such as age, male sex, and certain comorbidities play a similar role in RMD patients. PsA patients have a better outcome of SARS-CoV-2 infection compared to RA. The influence of disease activity is of great importance as patients in high disease activity – even without GCs – have a worse outcome. Regarding RMD treatment, patients on TNFi show a better outcome of SARS-CoV-2 infection than MTX patients. The negative impact of sulfasalazin shown in the global rheumatology alliance analysis [1] was not reproduced in this analysis. This might be due to the larger homogeneity in our data deriving from one country, resulting in less bias. The signals showing a less favorable outcome of SARS-CoV-2 infection for immunosuppressants, rituximab, and JAKi could be reproduced. These associations with a worse outcome of SARS-CoV-2 infection may be attributed to residual and unmeasured confounding due to higher burden of comorbidity or cumulative effect of therapies. However, the data show that the individual risk/benefit ratios for the different RMD treatments should be carefully considered and further evaluated.
CIs, assessing the association with (A) general patient characteristics, (B) comorbidities, (C) rheumatic disease diagnoses (RMD), (D) disease activity and glucocorticoids, and (E) rheumatic disease medications.
To cite this abstract in AMA style:
Regierer A, Hasseli R, Schaefer M, Hoyer B, Krause A, Lorenz H, Pfeil A, Richter J, Schmeiser T, Strangfeld A, Schulze-Koops H, Voll R, Specker C, Müller-Ladner U. Differential Impact of TNFi, JAKi and Rituximab on the Outcome of SARS-CoV-2 Infection in RMD Patients [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/differential-impact-of-tnfi-jaki-and-rituximab-on-the-outcome-of-sars-cov-2-infection-in-rmd-patients/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/differential-impact-of-tnfi-jaki-and-rituximab-on-the-outcome-of-sars-cov-2-infection-in-rmd-patients/