Session Information
Date: Friday, November 6, 2020
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Early diagnosis of psoriatic arthritis (PsA) is important for improving long-term outcomes. Trends in diagnostic delay of PsA in the US and factors associated with delay in diagnosis have not been well studied. The aim of our study was to 1) examine the diagnostic delay in PsA in residents of a geographically defined area from 2000-17, and 2) identify demographic and clinical characteristics associated with diagnostic delay in PsA.
Methods: A retrospective, population-based cohort of incident PsA patients ≥18 years of age from a geographically defined area meeting ClASsification of Psoriatic ARthritis (CASPAR) criteria for PsA (2000-17) was identified. Disease onset was taken as onset of any PsA related joint symptom as reported by the patient and documented by a physician in the medical records. PsA diagnosis date was the date of confirmatory diagnosis of PsA by a physician/rheumatologist. Diagnostic delay was defined as the time from disease onset to a diagnosis of PsA. Logistic regression models adjusted for age and sex were performed to identify factors associated with delay in PsA diagnosis.
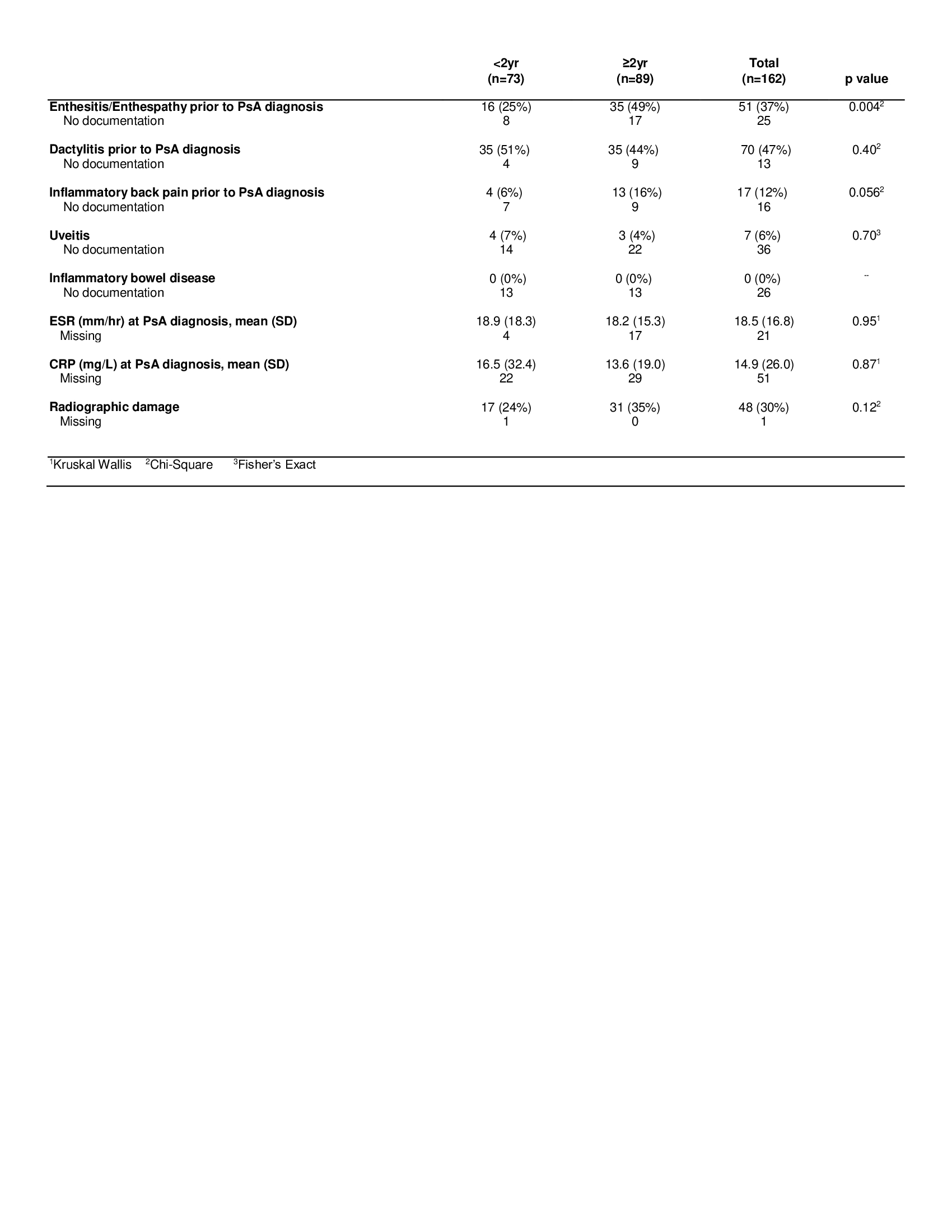
Results: There were 162 incident PsA cases from 2000-17. Mean age was 41.5 (SD=12.6) and 46% were females. Median lag time from disease onset (PsA related joint symptoms) to first confirmatory diagnosis by a physician was 2.5 years (interquartile range=0.5, 7.3). At six months 23% (n=38) of the cohort received a confirmatory diagnosis of PsA, 35% (n=56) at one year and 45% (n=73) at two years of symptom onset respectively. No significant trend in diagnostic delay were observed. PsA patients with younger age at diagnosis, higher body mass index (BMI), and enthesitis before diagnosis, were associated with a diagnostic delay of greater than one and two years, while sebopsoriasis at diagnosis was associated with a lower likelihood of delay (Table 1). No significant association with sex, education level, smoking status, alcohol intake, psoriasis severity or location, nail involvement, family history of psoriasis or PsA, history of extra-articular manifestations (i.e., uveitis, inflammatory bowel disease), or high inflammatory markers at the time of diagnosis was found. Logistic regression models adjusted for age and sex showed a higher likelihood of radiographic damage at PsA diagnosis with a delay in diagnosis of six months, one year and two years, however these associations did not reach statistical significance (Table 2).
Conclusion: In this population-based study, more than half of PsA patients had a delay in diagnosis two or more years, and no significant improvement in time to diagnosis was noted from 2000-17. Patients with younger age at diagnosis, higher BMI, or enthesitis before diagnosis were more likely to have a diagnostic delay of more than two years while patients with sebopsoriasis were less likely to have a diagnostic delay. Radiographic damage may be associated with diagnostic delay, but this association did not reach statistical significance, perhaps due to the limited sample size of the cohort.
 Table 1. Baseline characteristics of PsA patients with delay in diagnosis < 2 years compared to ≥2 years
Table 1. Baseline characteristics of PsA patients with delay in diagnosis < 2 years compared to ≥2 years
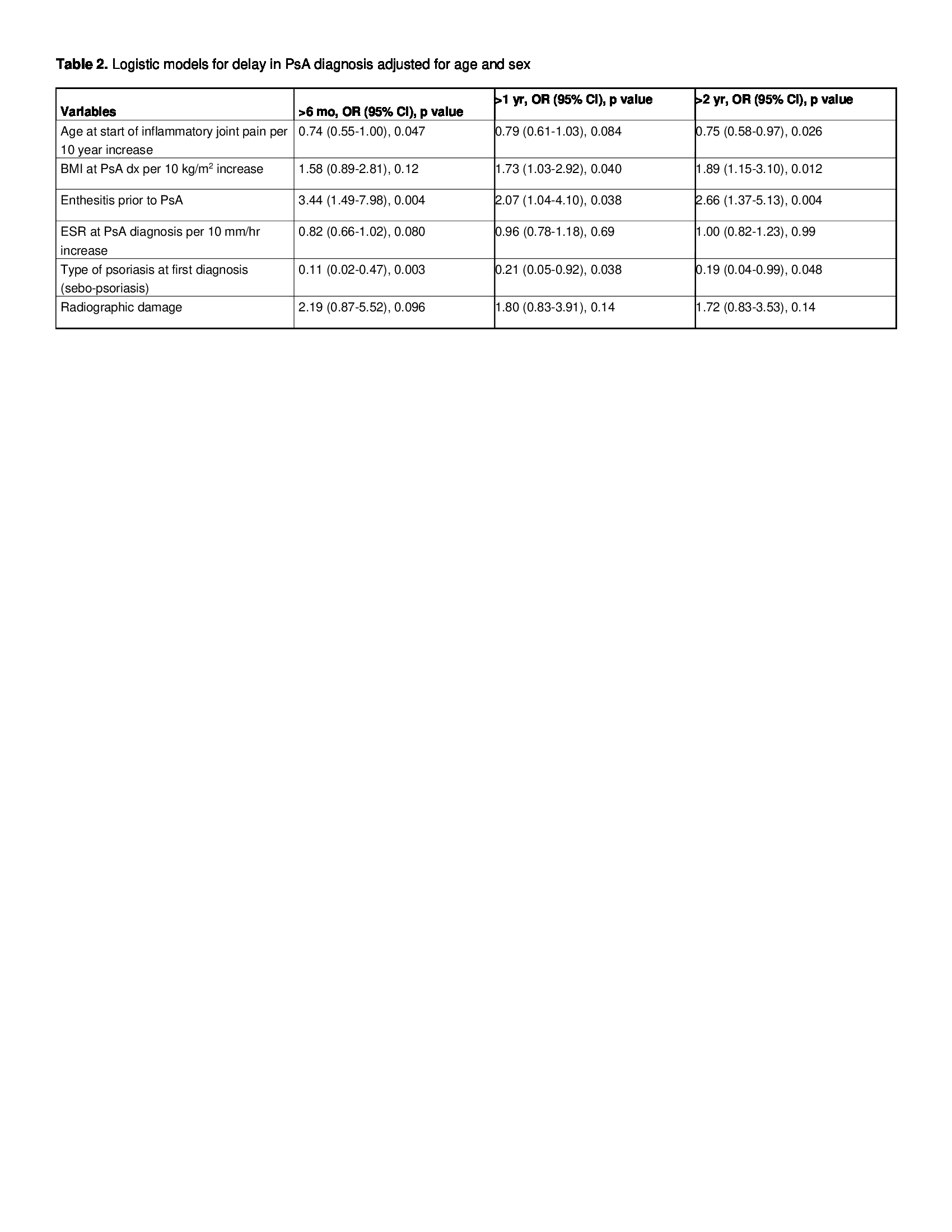 Table 2. Logistic models for delay in PsA diagnosis adjusted for age and sex
Table 2. Logistic models for delay in PsA diagnosis adjusted for age and sex
To cite this abstract in AMA style:
Karmacharya P, Wright K, Achenbach S, Bekele D, Crowson C, Ogdie A, Duarte-Garcia A, Ernste F, Tollefson M, Davis J. Diagnostic Delay in Psoriatic Arthritis: A Population Based Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/diagnostic-delay-in-psoriatic-arthritis-a-population-based-study/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/diagnostic-delay-in-psoriatic-arthritis-a-population-based-study/