Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
Vasculopathy is a major feature of systemic sclerosis (SSc). It leads to intimal proliferation and adventitial fibrosis of small and large arterial blood vessels. Videocapillaroscopy (VC) for nailfold-capillaries and MR-angiography (MRA) for arteries are established methods to assess pathologies. However, little is known about the correlation between VC and MRA and about the evolution of changes in response to therapy over time.
Methods:
We included consecutive patients of our tertiary center who had a MRA between 1.1.2008 – 30.04.2018. We present an intermediate analysis performed in 03/2015: twenty-one patients with SSc (mean age 55.2±15.6; 13 females, 8 males; 4 diffuse SSc, 17 limited SSc) and 22 patients with other inflammatory rheumatic diseases (OD; mean age 50.1±18.8; 15 females, 7 males) had a total of 71 MRA acquired by a 3T MR scanner. We analyzed digital arteries and calculated a semiquantitative vascular score. We compared the MRA with the VC in correlation with clinical and laboratory data. We further analyzed a subgroup of 8 patients who had both a MRA and VC twice or more. We used SPSS version 23 program, Pearson’s Chi-Test, Fisher’s test for statistics.
Results:
ANA were significantly more frequent in SSc- (85%) than in OD-patients (50%) (p<0.001), ACA in 38% and 10% (p 0.02), Scl70 in 38% and 4% (p<0.001) respectively. Raynaud was present in 95% of SSc patients and 61% in OD, DU in 71.4% and 73.5% respectively. Duration of Raynaud was significantly longer (p 0.005) in limited vs diffuse form (72.2 vs 30 months). However, prevalence of DU was similar in both limited and diffuse SSc.
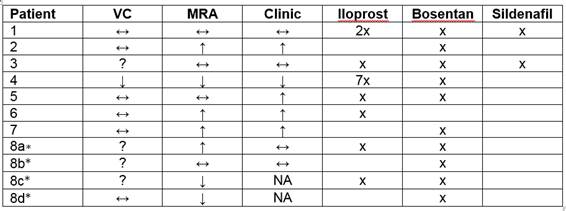
The subgroup analysis of patients with 2 or more pairs of VC/MRA are showed in table 1.
In 7 out of 11 cases, the clinical changes correlated with MRA changes, in 2 cases they didn’t; 2 cases cannot be analyzed because of missing data. VC only correlated with the clinical course in 2 cases, while 5 cases had missing or unclear data. VC status did not improve, even if the clinical status did. Two patients with OD and 2 of 6 with SSc showed clinical improvement.
In case of DU, there was a good correlation with vessel damage, but damaged vessels did not necessarily result in DU of the corresponding finger.
Table 1: Course of VC, MRA and clinical status in a subgroup of 8 patients. ↔ stable status; ↑ better status; ↓ worse status; * the patient 8 had 5 pairs of VC/MRA; each letter depicts the course between two such pairs; x the patient had the medication mentioned above. NA not available; ? status could not be interpreted
Conclusion:
MRA assesses reliably and accurately the vasculopathy of the hand in SSc. It may unveil important subclinical vessel damage and bears the potential to guide preventive drug treatment. Unlike VC, MRA appears to correlate with the clinical course.
To cite this abstract in AMA style:
Dan D, Saner S, Gloor AD, Bonel H, Cullmann JL, Villiger PM. Diagnostic Accuracy of MR Angiography in a Cohort with Systemic Sclerosis Compared to Other Rheumatic Diseases with Acral Hypoperfusion [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/diagnostic-accuracy-of-mr-angiography-in-a-cohort-with-systemic-sclerosis-compared-to-other-rheumatic-diseases-with-acral-hypoperfusion/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/diagnostic-accuracy-of-mr-angiography-in-a-cohort-with-systemic-sclerosis-compared-to-other-rheumatic-diseases-with-acral-hypoperfusion/