Session Information
Session Type: ARHP Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Individuals with specific comorbid conditions have increased risk of having hip osteoarthritis (OA). Some of these conditions are also associated with increased risk of premature death. In this study, we explored diabetes (DM) and body mass index (BMI) as modifiers of the association between hip OA measures and all-cause death.
Methods: We analyzed data from the Johnston County Osteoarthritis Project to investigate the association between baseline radiographic hip OA (rOA) and all-cause death, stratified by DM and BMI. Analyses were carried out using baseline data from 2,381 individuals with hip radiographs, including men aged 45 or older and women over 50 who entered the cohort during the original study enrollment (1990-1997; n=1,817) and those with their baseline assessment during the cohort enrichment (2003-2004; n=564). Vital status was assessed using National Death Index records to capture date of death. Person-years of follow-up were accrued from baseline assessment to the date of death, loss to follow-up or December 31, 2014, whichever came first. Hip rOA was defined as a Kellgren-Lawrence (KL) grade of ≥2 in either hip at baseline clinical assessment. Symptomatic rOA (sxOA) is a subset of those with rOA who also had symptoms of pain in the same joint. We used multivariable Cox proportional hazards regression models to estimate hazard ratios and 95% confidence intervals for the risk of all-cause mortality. Interactions by BMI group (<25, 25-<30, ≥30) and self-reported DM (yes/no) at baseline were assessed at the p=0.1 level.
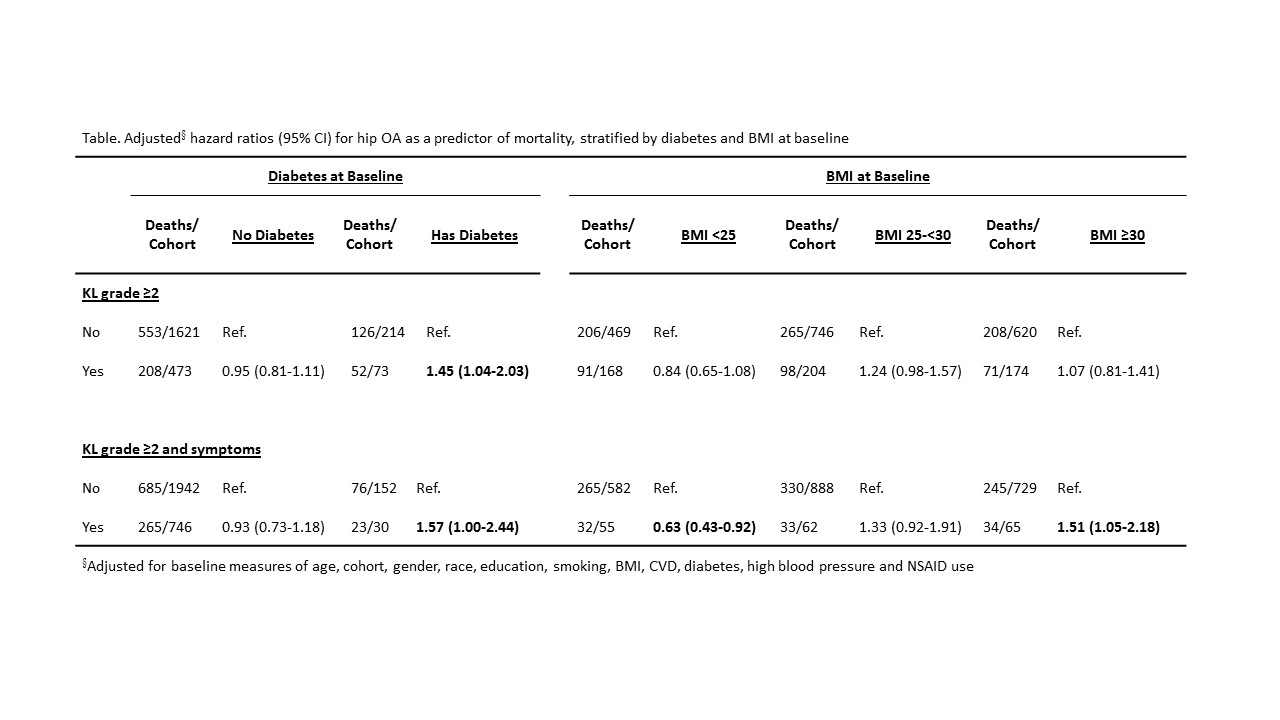
Results: At baseline, the mean age was 61.1 years; 55.9% were women, 31.5% African American, 33.3% did not complete high school, 23.8% were smokers. There were 12.0% with DM and 33.4% had a BMI≥30. Mean follow-up time was 14.2 (SD=5.7) years. Adjusted HRs for the association of hip rOA and sxOA with death were higher among individuals with DM at baseline (Table). We observed interactions on the multiplicative scale for hip rOA with a KL grade ≥2 (interaction p=0.015) where those with DM and hip OA were 45% more likely to die than those without hip OA, whereas we observed no association between hip rOA and death among those without DM. A similar association was observed among those with hip sxOA (interaction p=0.018). Further, among those with a BMI≥30, we observed a 50% increase in hazards for the association of hip sxOA on mortality, no association with BMI 25-<30 and reduced hazards for BMI<25 (interaction p<0.001).
Conclusion: The associations between hip OA measures and mortality were increased among those with DM and higher BMI at baseline. These associations were particularly strong among those with symptomatic disease and were independent of other comorbidities and sociodemographic measures. Our results suggest roles for DM and BMI in the link between hip OA and mortality, findings that merit further investigation into potential mechanisms and clinical attention.
To cite this abstract in AMA style:
Cleveland R, Schwartz TA, Renner JB, Callahan LF, Jordan JM. Diabetes and BMI Modify the Association Between Painful Hip OA and All-Cause Mortality [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/diabetes-and-bmi-modify-the-association-between-painful-hip-oa-and-all-cause-mortality/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/diabetes-and-bmi-modify-the-association-between-painful-hip-oa-and-all-cause-mortality/