Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Little is known on the development of spondyloarthritis (SpA)-features over time in patients with recent onset chronic back pain (CBP). The aim was to explore whether patients with suspicion of axial spondyloarthritis (axSpA) develop SpA-features over time in the SPACE-cohort, and to study the effect of gaining features on the clinical diagnosis and classification according to the Assessment of SpondyloArthritis international Society (ASAS)-criteria for axSpA.
Methods: SPACE is an inception cohort study in which CBP patients ( ≥ 3 months, ≤ 2 years, onset < 45 years) from various rheumatology centres across Europe are included. Baseline (BL) and one-year (FU) data were used for this study. Patients underwent a full diagnostic work-up consisting of MRI and radiographs of the sacroiliac joints (MRI-SI and X-SI), acute phase reactants, HLA-B27, and assessment of all other SpA-features. For the purpose of this study positive SpA-features were accumulated according to the principle of “once a feature always a feature” meaning patients were not able to ‘lose’ features over time. Total number of SpA-features was calculated excluding sacroiliac imaging and HLA-B27 status. Clinical diagnosis (axSpA yes/no) of patients was provided by the treating rheumatologist with use of local reading and the ASAS-criteria for axSpA (based on central scoring and agreement of 2/3 readers) were used for classification.
Results: A total of 270 patients with CBP with both baseline and one-year follow-up visits were included: 36.7% were male, mean age (SD) at inclusion was 31.2 (8.0) years, mean number of SpA-features (SD) at BL and one-year FU were 2.8 (1.5) and 3.5 (1.6), respectively. After one year 49.3% of patients had gained one or more features. Most common features were IBP (BL: 77.0%, FU: 88.2%), good response to NSAIDs (BL: 48.5%, FU: 70.6%), elevated CRP/ESR (BL: 29.5%, FU: 43.3%), and positive family history for SpA (BL: 48.9%, FU: 52.6%). For 16 out of the 270 patients information on diagnosis at either BL or FU was missing. In the remaining 254 patients, rheumatologists diagnosed 150 (59.1%) and 66 (26.0%) patients with axSpA and no axSpA at both time points, respectively (Figure 1). In 15.0% (38/254) of patients the diagnosis changed; 16 patients with no axSpA diagnosis at BL were diagnosed with axSpA at FU of which 11/16 (68.8%) had acquired one or more features. In 22 patients with axSpA at BL rheumatologists reconsidered their diagnosis at FU. In the 150 patients diagnosed with axSpA, 108/150 (72%) of patients already fulfilled the ASAS-criteria at BL and 79/150 (52.7%) patients gained a minimum of one feature, which led to a new axSpA classification for 9 patients at FU.
Conclusion: In patients with CBP of short duration almost half developed at least one new SpA-feature within one year, however the impact on diagnosis and classification was limited. 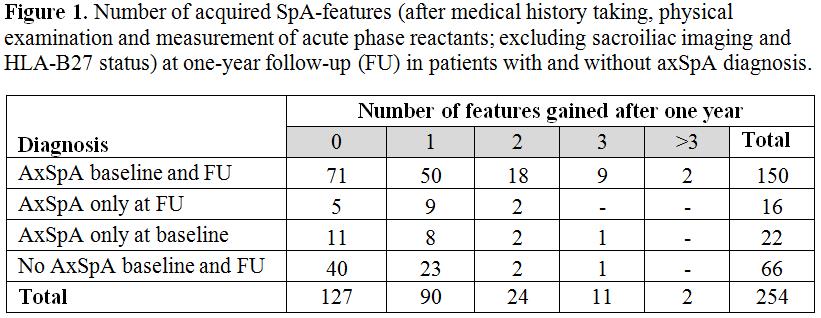
To cite this abstract in AMA style:
Ez-Zaitouni Z, van Lunteren M, Bakker P, Berg IJ, Landewé R, van Oosterhout M, Ortolan A, van der Heijde D, van Gaalen F. Development of Spondyloarthritis-Features in Patients with Chronic Back Pain over a One-Year Course: Data from the Spondyloarthritis Caught Early (SPACE)-Cohort [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/development-of-spondyloarthritis-features-in-patients-with-chronic-back-pain-over-a-one-year-course-data-from-the-spondyloarthritis-caught-early-space-cohort/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/development-of-spondyloarthritis-features-in-patients-with-chronic-back-pain-over-a-one-year-course-data-from-the-spondyloarthritis-caught-early-space-cohort/
