Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Osteoporosis is a major public health concern in the United States, leading to significant morbidity, mortality, and increased economic burden. Fractures are projected to exceed 3 million at a cost of over $25 billion by 2025. Screening for osteoporosis reduces fracture incidence. Thus, prioritizing screening is essential to lower healthcare costs and improve the quality of life for high-risk patients.
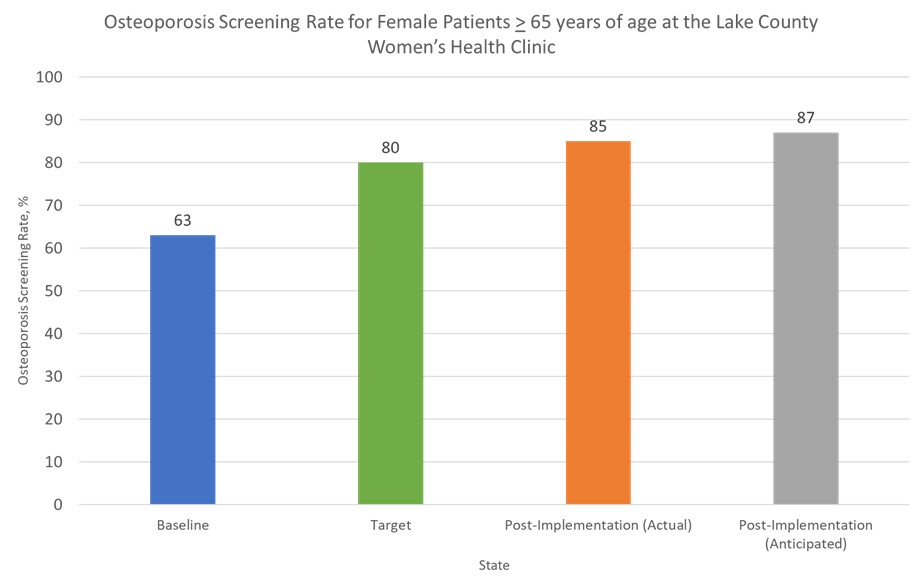
Osteoporosis screening rates are suboptimal within the VA NEOhio Healthcare System (VANEOHS). Despite a clinical reminder to order DXA scans, primary care clinics only screen 44% of eligible female patients, compared to 90% in non-VA clinics. This quality improvement project aimed to identify barriers to osteoporosis screening throughout the VANEOHS and implement an intervention to improve the screening rate from 63% to 80% in a VA Women’s Health (WH) clinic over 1 year.
Methods: Our team, consisting of clinical pharmacists, physicians, and a Lean Six Sigma coach conducted a quality improvement study in several phases.
- Define: we determined a system-wide screening rate by identifying female patients over 65 with a documented DXA scan or diagnosis of osteoporosis/osteopenia coded in the electronic medical record (EMR).
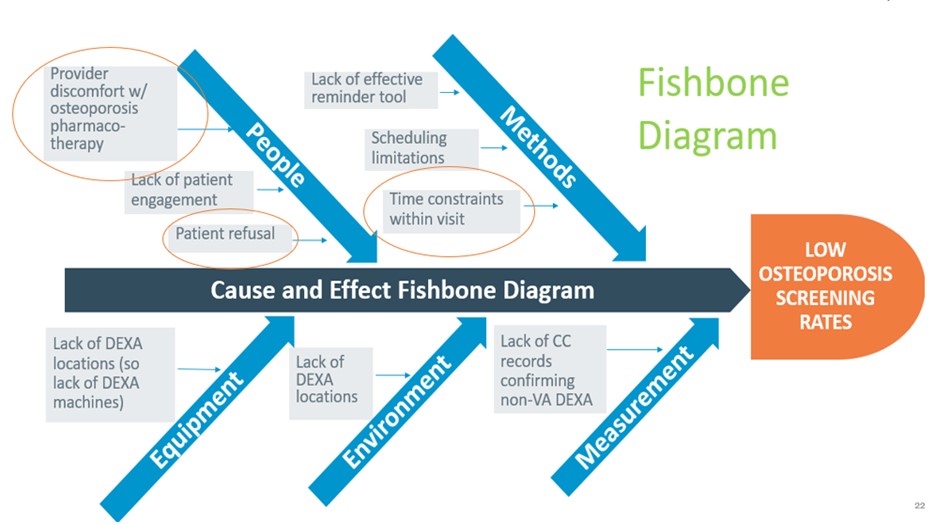
- Measure and Analyze: we observed patient visits, sent a survey to 100 primary care providers regarding barriers to screening, the utility of the EMR reminder, and comfort with involving clinical pharmacists in osteoporosis care, and completed a root cause analysis (RCA) to identify areas for process improvement.
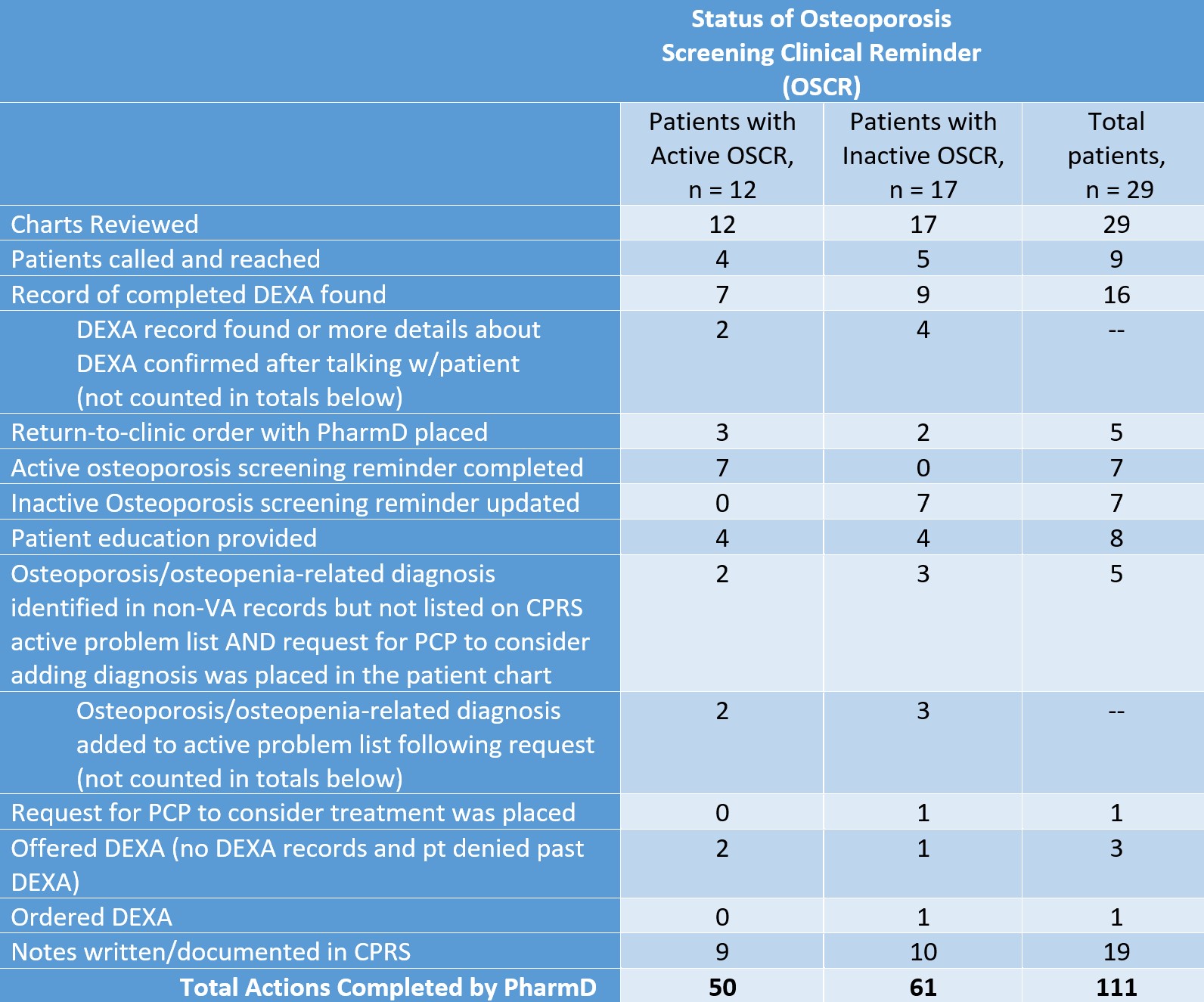
- Improve: we used pharmacy-driven solutions to address physician-reported barriers and tested their impact on a small scale. At a single VA Women’s Health clinic, pharmacists identified eligible patients, reviewed records, updated documentation, provided education, ordered DXAs, and scheduled follow-ups. We tracked these actions and calculated a final screening rate after 60 days.
Results:
- Define: 44% (653/1492) of eligible females in VA primary care clinics had a DXA scan completed at the VA. Of those with qualifying ICD diagnoses (351), only 244 had a DXA scan.
- Measure and Analyze: the provider survey response rate was 20%. 50% of respondents found the EMR reminder helpful, and 50% were willing to consult pharmacists. Physician time constraints, prioritization of other conditions, and discomfort with managing osteoporosis were the most common barriers to screening, as identified in the RCA.
- Improve: we calculated an initial screening rate of 63% based on 55 of 87 eligible patients enrolled at our intervention site with a documented DXA or qualifying ICD diagnosis. We eventually excluded 3 patients determined to be ineligible due to death, male sex, and loss of VA services. Pharmacists took over 100 actions for the remaining patients, resulting in a final screening rate of 85% (71/84).
Conclusion: Our study addressed gaps in osteoporosis care with key pharmacist-driven interventions allowing for comprehensive record review and direct patient engagement while also reducing physician workload. Our results demonstrate the impact of a multidisciplinary approach to care and the potential for this model to improve screening-based care in settings beyond the VA.
To cite this abstract in AMA style:
Topalsky K, Arphai L, Amos M, Mertz A, Blum C, Godbey T, Leonard L, Mattar M, Cable E, Wenzell R. Development of a Pharmacy-Led Intervention to Improve Osteoporosis Screening in VA Community-Based Outpatient Clinics [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/development-of-a-pharmacy-led-intervention-to-improve-osteoporosis-screening-in-va-community-based-outpatient-clinics/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/development-of-a-pharmacy-led-intervention-to-improve-osteoporosis-screening-in-va-community-based-outpatient-clinics/