Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Adherence to systemic therapies, such as tumor necrosis factor inhibitors (TNFi’s), is affected by various factors and may be critical for optimal disease outcomes in patients (pts) with inflammatory diseases such as ankylosing spondylitis (AS). An adherence prediction model may help rheumatologists identify pts with AS at high risk of non-adherence to systemic therapies.
Methods: The global cross-sectional non-interventional ALIGN study enrolled >7000 adult pts with 6 immune-mediated inflammatory diseases, including AS as diagnosed by treating physician, currently being treated with conventional systemic therapies and/or TNFi’s. Validated questionnaires, including the 4-item Morisky Medication Adherence Scale (MMAS-4©) and the Beliefs about Medicines Questionnaire (BMQ), were administered to pts at a routine visit. The objective of this analysis was to identify an accurate adherence prediction model by 1) identification of factors significantly associated with high medication adherence (MMAS-4 = 4) in multiple regression analysis based on backward selection and dichotomization of quantitative variables for simplicity reasons, 2) selection of the model, consisting of up to 10 variables, with the highest cross-validated area under the receiver operating characteristic curve (AUROC), and 3) visual representation of certain pt profiles in the adherence probability matrix based on the best model.
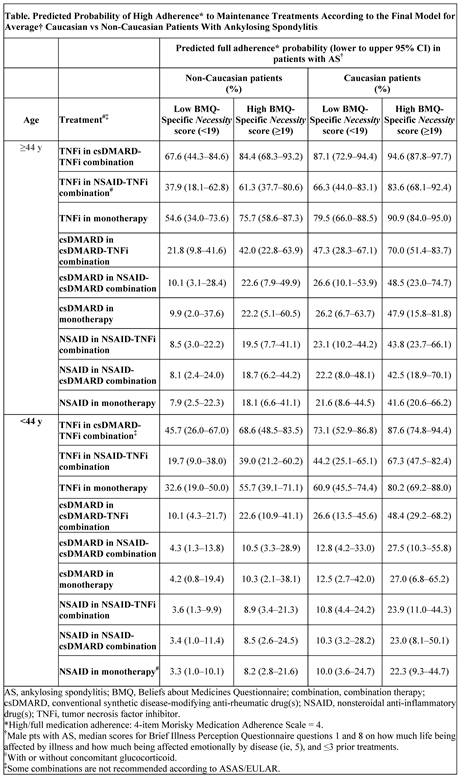
Results: A total of 812 pts with AS were analyzed (mean age, 42.5 y; disease duration, 9.3 y; prior TNFi therapy, 51%; male, 71%). Based on MMAS-4 items, more pts with csDMARD or NSAID vs TNFi monotherapy admitted forgetting to take their medication (32 ̶ 49% vs 18%) or stopping medication when feeling better (20 ̶ 48% vs 17%). The best model had an AUROC of 0.7492 and included the following variables: age, ethnicity, sex, type of treatment, medication necessity beliefs (BMQ-Specific Necessity score), illness perception (Brief Illness Perception Questionnaire scores), and number of prior treatments. According to the model, the highest predicted probability of full adherence was seen in pts with AS ≥44 years of age, with high treatment necessity beliefs and TNFi treatment (especially in combination; Table). The predicted probability of full adherence was higher in Caucasian pts compared with non-Caucasian pts with the same characteristics.
Conclusion: Results from the first medication adherence prediction model for pts with AS suggest that the majority of pts with NSAID or csDMARD treatment are not completely adherent to their therapy. The developed prediction model visualizes the impact of factors on medication adherence in pts with AS, which could help clinicians identify pts at high risk of non-adherence to systemic treatment. Further studies need to confirm the developed model.
To cite this abstract in AMA style:
Mease PJ, Smolen JS, Gladman DD, Sieper J, Weinman J, Sommer J, Nurwakagari P, Hojnik M. Development of a Novel Medication Adherence Prediction Model for Patients with Ankylosing Spondylitis Based on Results from a Global Clinical Study [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/development-of-a-novel-medication-adherence-prediction-model-for-patients-with-ankylosing-spondylitis-based-on-results-from-a-global-clinical-study/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/development-of-a-novel-medication-adherence-prediction-model-for-patients-with-ankylosing-spondylitis-based-on-results-from-a-global-clinical-study/