Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: Hydroxychloroquine (HCQ) is an important medication for SLE and other rheumatic diseases, but its major adverse event is HCQ retinopathy. Weight-based HCQ dose is known to influence the risk of retinopathy, but other risk factors have also been identified. We explored predictive models for HCQ retinopathy and developed a clinical risk score.
Methods: We used a longitudinal cohort of incident HCQ users enrolled in the United States integrated health network Kaiser Permanente Northern California. HCQ retinopathy outcomes were obtained by masked expert-adjudication of optical coherence tomography screening studies, as previously described (Melles RB, Jorge A, Ann Int Med 2023). Among patients using HCQ for at least 5 years, we assessed candidate predictors at 5 years of use including the weight-based HCQ dose, cumulative dose in the first 5-years, age, sex, race/ethnicity, biometrics, indication for HCQ use, comorbidities including diabetes, liver disease, estimated glomerular filtration rate (eGFR), tamoxifen use, and use of inhibitors of cytochrome P450 CYP2D6, CYP2C8, or CYP3A4. We used Cox proportional hazards regression, using backwards stepwise selection to develop a parsimonious model, and an alternate method of random survival forest (RSF) to identify predictors of the 10-year risk of HCQ retinopathy (i.e., risk within 15 years from HCQ initiation). We created a comparator model using HCQ dose alone (weight-based dose at 5 years: > or ≤ 5 mg/kg). We assessed model discrimination with c-statistics, assessed model calibration using the Hosmer-Lemeshow statistic, and graphed deciles of predicted vs observed risk. We then developed an integer-based risk score from the optimal Cox model. Continuous variables were converted to categorical variables. We assessed net reclassification improvement and integrated discrimination improvement between the integer-based risk score and comparator model with HCQ dose alone.
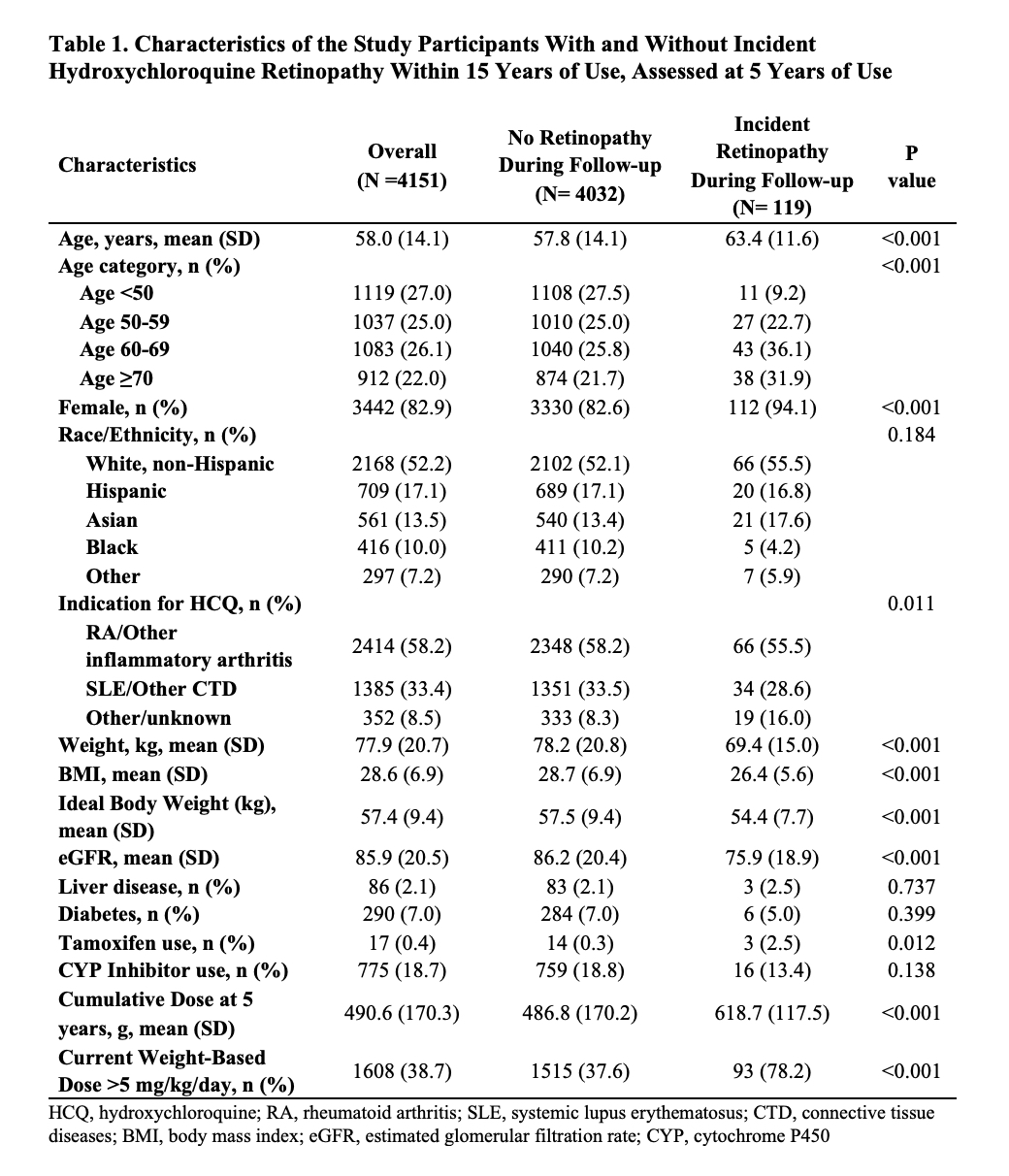
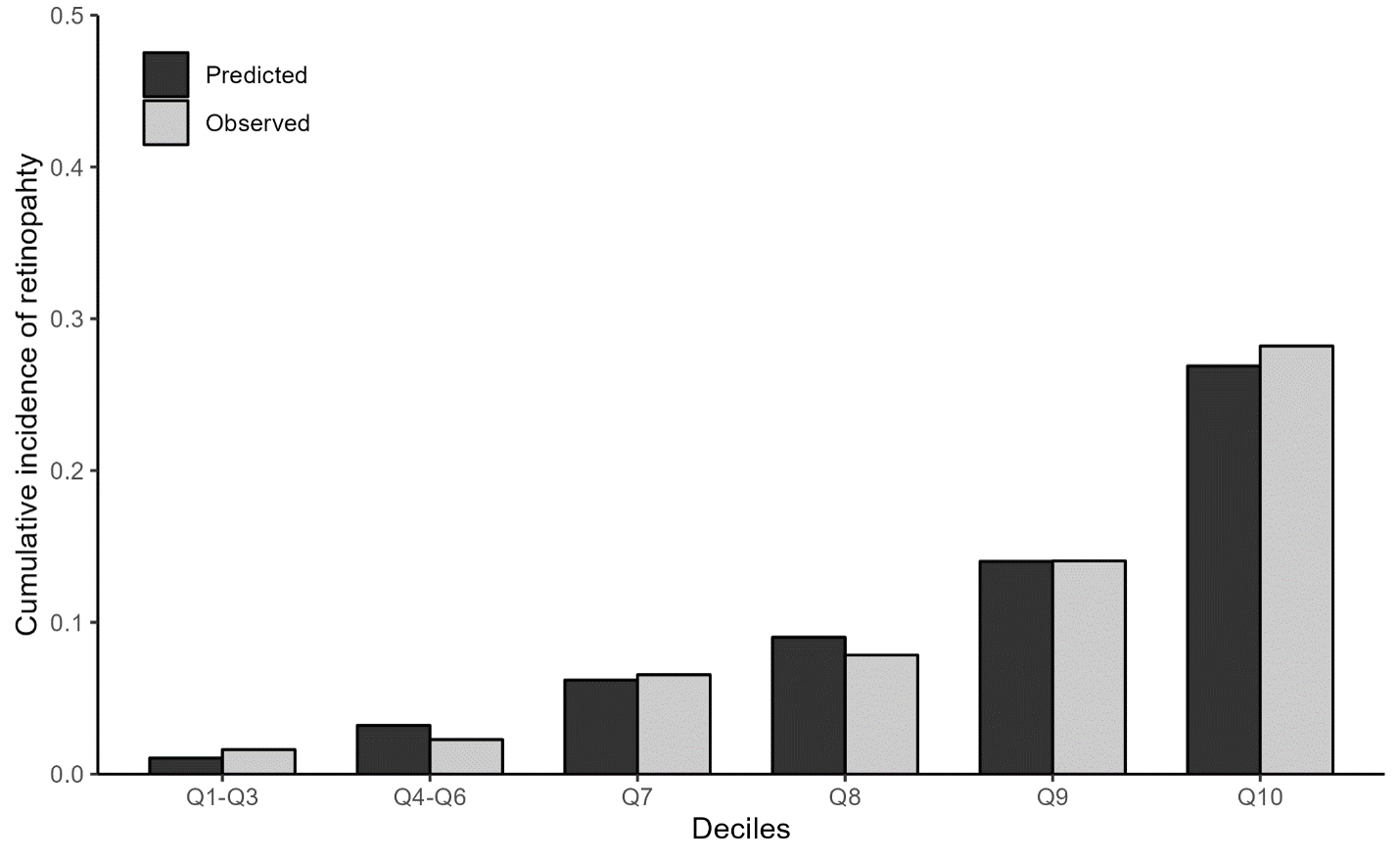
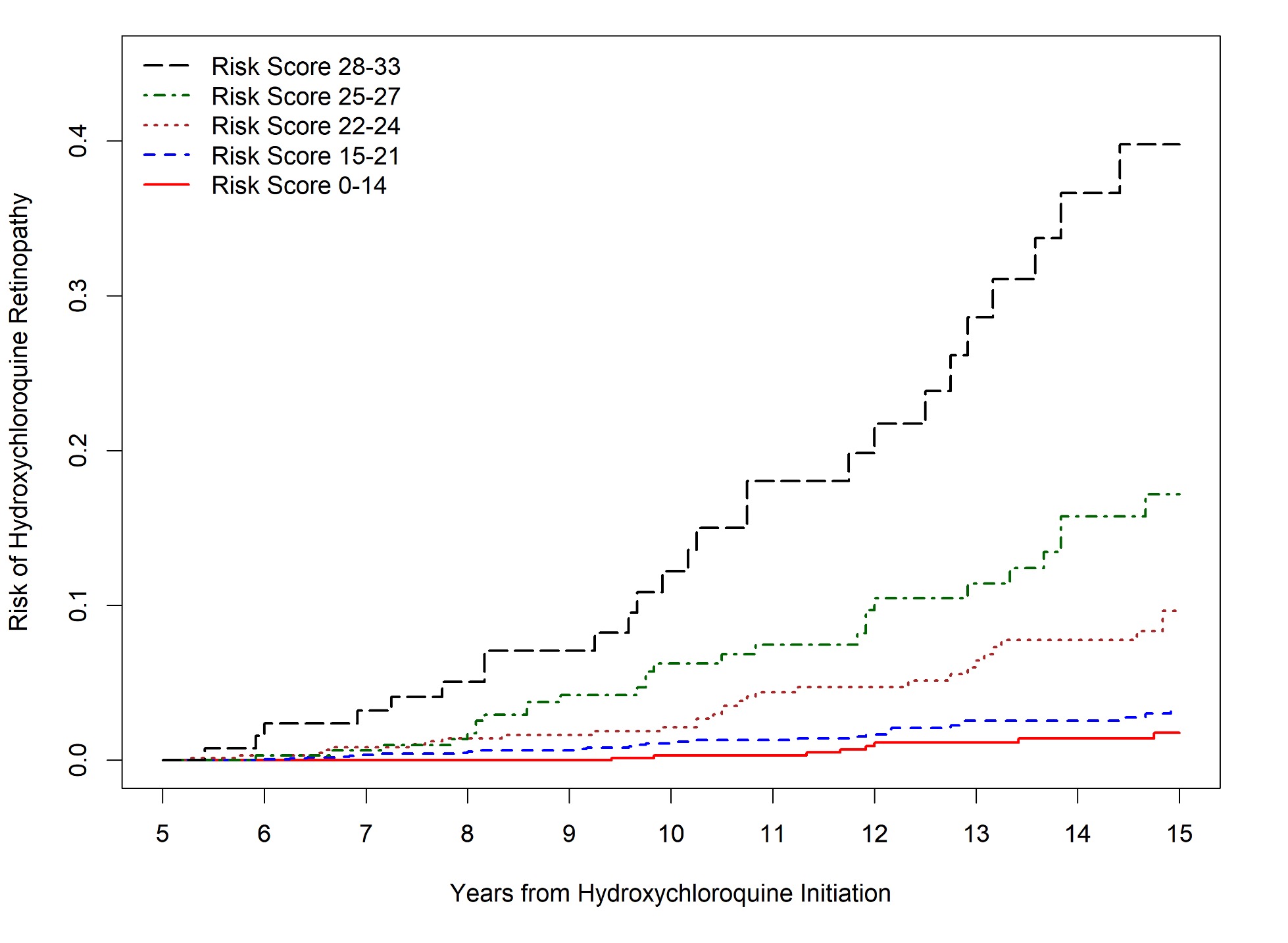
Results: Of 4,151 patients who initiated HCQ and continued for ≥5 years, 119 developed HCQ retinopathy within 15 years (Table 1). The final Cox model had better discrimination than the RSF model and than HCQ dose alone (C-statistic 0.80 [95% CI 0.77-0.83] versus 0.62 (95% CI 0.53-0.70) for the RSF model and 0.72 [95% CI 0.68-0.77] for the HCQ dose-only model. From the identified predictors in this model, an integer-based risk score for 10-year risk of HCQ retinopathy was created: B-SAFE (Body weight [kg], Sex, Age, glomerular Filtration rate, Exposure (cumulative dose in first 5 years since initiation [g] and current weight-based dose [mg/kg/day]). The B-SAFE model c-statistic was 0.78 (95% CI 0.75=0.82) with acceptable calibration (Figure 1). Compared with the HCQ dose-only model, the net reclassification index was 0.34 (95% CI 0.20-0.46). The risk score ranged from 0-33 points and can identify patients with HCQ retinopathy risk ranging from < 1% to >20% (Figure 2).
Conclusion: In addition to weight-based HCQ dose, we identified additional predictors of HCQ retinopathy. These clinical and laboratory variables were incorporated into a novel risk score that performs better than HCQ dose alone in predicting the 10-year risk of HCQ retinopathy among long-term users.
To cite this abstract in AMA style:
Jorge A, Melles R, Zhou B, Zhang Y, Choi H. Development of a Hydroxychloroquine Retinopathy Prediction Score [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/development-of-a-hydroxychloroquine-retinopathy-prediction-score/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/development-of-a-hydroxychloroquine-retinopathy-prediction-score/