Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Psoriatic arthritis (PsA) is a chronic, progressive inflammatory disease of the skin and musculoskeletal system, affecting over half a million US adults. With relatively uncommon diseases such as PsA, electronic health records (EHR) offer an opportunity to better understand long-term outcomes in the real-world setting. EHR are an efficient and cost-effective tool that allows for the identification of a large number of patients in the real-world setting for clinical and translational research. However, the clinical heterogeneity of PsA along with a lack of clear diagnostic criteria or tests poses a diagnostic challenge. This also translates into a difficulty in identifying PsA patients in the EHR. Identifying PsA patients accurately in the EHR is crucial to study long-term outcomes in PsA in the real-world setting. Therefore, the objective of this study was to develop EHR algorithms to accurately identify patients with PsA.
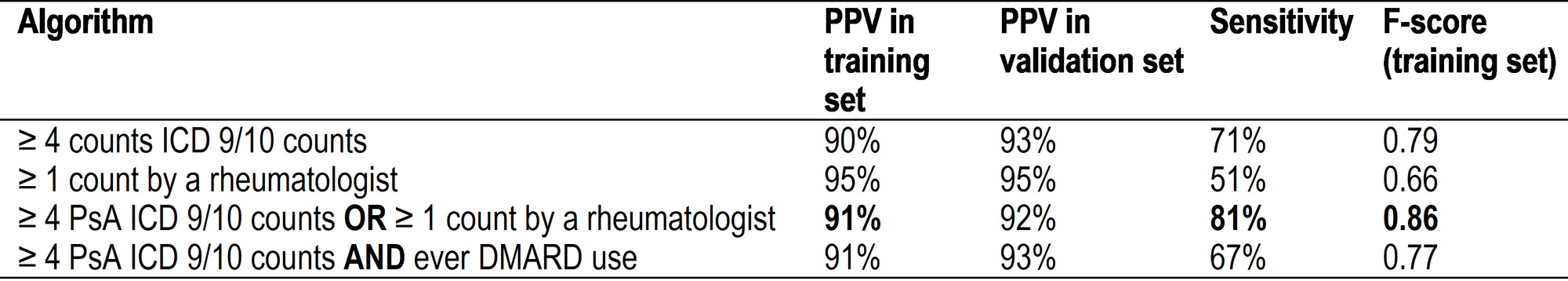
Methods: We used a de-identified version of Vanderbilt’s EHR called the Synthetic Derivative (SD containing ~3.5 million subjects) to identify our PsA cohort. The SD includes longitudinal clinical data over several decades (1993-2021) with all information available in the EHR. We screened the SD for adult patients (≥18 years of age) with one International Classification of Diseases, Ninth or Tenth Revision (ICD 9/10) code for psoriatic arthritis or any psoriatic arthritis keyword in the problem list (Figure 1). Of the 5,636 potential PsA cases, we randomly selected 200 for chart review to identify their true disease status and to serve as a training set and a separate random set of 300 as the validation set. A rheumatologist diagnosis of PsA or fulfillment of CASPAR criteria based on manual chart review was used as the reference standard. Potential algorithm components decided a priori were ICD 9/10 codes for PsA and psoriasis, ICD 9/10 codes for PsA by rheumatology and dermatology, keywords for PsA in the problem list, and use of disease-modifying antirheumatic drugs (DMARDs). Positive predictive value (PPV) and sensitivity, along with the F-score (harmonic mean of PPV and sensitivity), were calculated.
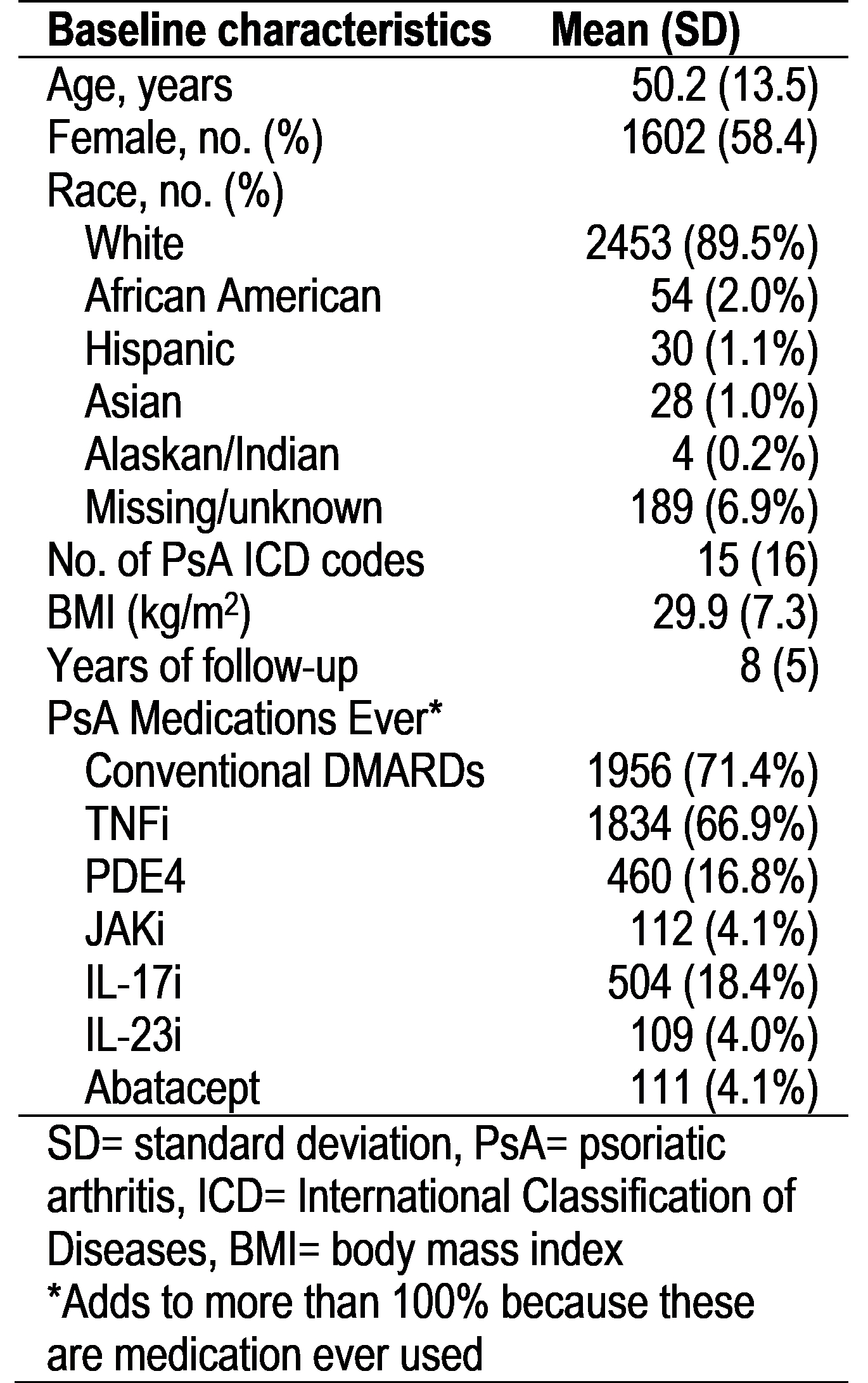
Results: The best-performing algorithms in the training and validation sets are shown in Table 1. Using the best performing algorithm of ≥ 4 PsA ICD 9/10 codes OR at least 1 ICD 9/10 code by a rheumatologist (PPV of 91%, sensitivity 81%, F-score 0.86), we identified 2,742 PsA patients. The mean age of the EHR cohort was 50.2 (SD 13.5), 58.4% female, and the majority (89.5%) were white, with a mean follow-up of 8 (SD 5) years (Table 2).
Conclusion: We have successfully developed an EHR algorithm using ICD-9/10 codes, demonstrating a PPV of 92% in internal validation. This rule-based algorithm represents a useful tool for clinical and translational research to identify PsA patients efficiently and accurately in an EHR. The EHR-based PsA cohort will enable longitudinal, de-identified chart review for further sub-phenotyping, and pragmatic clinical studies that pave the way for personalized treatment approaches.
To cite this abstract in AMA style:
Karmacharya P, Fortier A, Sellyn G, Ogdie A, Crofford L. Developing Electronic Health Record Algorithms to Accurately Identify Psoriatic Arthritis Patients [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/developing-electronic-health-record-algorithms-to-accurately-identify-psoriatic-arthritis-patients/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/developing-electronic-health-record-algorithms-to-accurately-identify-psoriatic-arthritis-patients/