Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Antiphospholipid syndrome (APS) is a heterogeneous disease, with different phenotypes which may widely vary from classical thrombotic or obstetrical manifestations to catastrophic antiphospholipid syndrome (CAPS). APS can be associated with other auto-immune diseases, such as systemic lupus erythematosus (SLE). We aimed to determine distinct homogenous phenotypes among APS patients, using a non-supervised hierarchical cluster analysis.
Methods: We performed an observational, retrospective study on APS patients satisfying Sydney classification criteria and enrolled in the French multicentre “APS and SLE” registry. The clustering process involved an unsupervised multiple correspondence analysis followed by hierarchical ascendant clustering analysis, using 27 selected variables to widely cover APS clinical and biological manifestations. Comparisons between different subgroups were performed with Chi-2 tests and ANOVAs.
Results: We included 509 patients in the analyses, mainly women (78%). Mean (± SD) age at APS diagnosis was 36.3 ± 14.7 years, and mean follow-up duration after APS diagnosis was 10.3 ± 8.5 years. Cluster hierarchical classification yield in four homogenous groups of patients. Their main characteristics are described in Table 1.
- Cluster 1 (n=181) included mostly patients with venous thrombosis (78%) and premature births due to placenta insufficiency (14%) history, without associated auto-immune disease (only 2.2%).
- Cluster 2 (n=130) included older patients (mean 45.8 years), less frequently women (65% of women), with arterial events history (89%). Valvular involvement (21%), migraine (21%), livedo (35%), arterial hypertension (49%), and cardiovascular risk factors were relatively frequent.
- Cluster 3 (n=102) included younger patients, frequently women (mean 30.7 years; 92% women), with associated SLE (76%) or other autoimmune diseases (30%). They frequently had history of venous thrombosis (74%) and of pregnancy morbidity (36%). Thrombocytopenia (48%), haemolytic anaemia (14%), and lupus anticoagulant (84%) were frequent.
- Cluster 4 (n=96) included mainly patients with a history of CAPS (77%) and/or APS-associated nephropathy (93%), and pregnancy morbidity (36%). Renal hypertension (61%), livedo (36%), seizures (14%), valvular involvement (44%) and triple positivity (66%) were relatively frequent.
Conclusion: Using an unsupervised clustering method, our study highlighted four distinct homogenous subgroups of APS patients that were predominantly venous; arterial; associated with SLE or other autoimmune disease; and microthrombotic. It confirms the underlying idea of heterogeneous pathophysiological mechanisms.
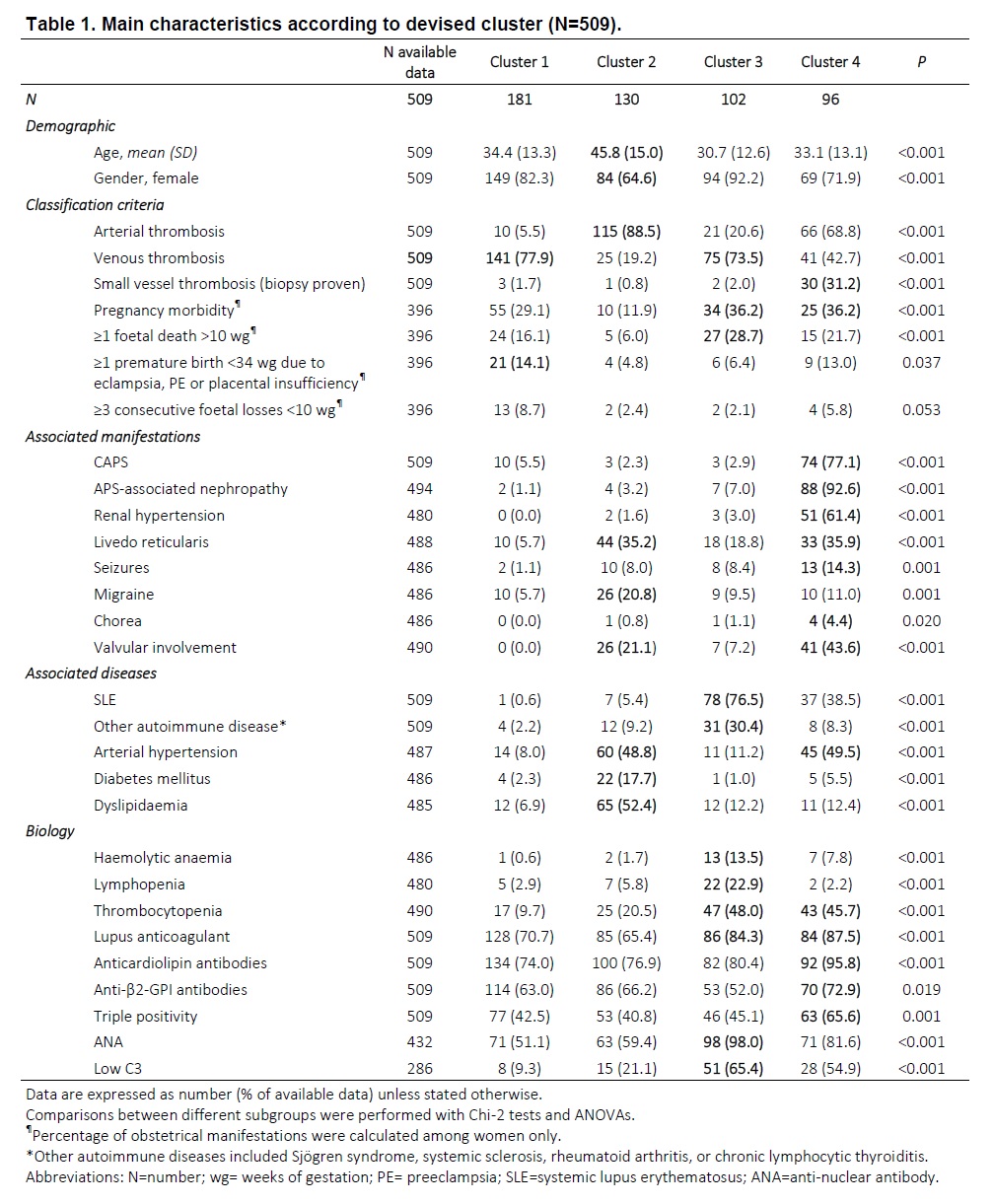 Table 1. Main characteristics according to devised cluster (N=509).
Table 1. Main characteristics according to devised cluster (N=509).
To cite this abstract in AMA style:
Nguyen Y, Yelnik C, Morel N, Paule R, Hatron P, Stammler R, Plaçais L, Piette J, Mouthon L, Hachulla E, Lambert M, Véronique L, Costedoat-Chalumeau N. Determination of Homogenous Subgroups of Antiphospholipid Syndrome: A Cluster Analysis Based on 509 Cases [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/determination-of-homogenous-subgroups-of-antiphospholipid-syndrome-a-cluster-analysis-based-on-509-cases/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/determination-of-homogenous-subgroups-of-antiphospholipid-syndrome-a-cluster-analysis-based-on-509-cases/
