Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The clinical heterogeneity of psoriatic arthritis (PsA) presents a variety of diagnostic and treatment challenges, which may be reflected in the way different health care providers approach the treatment of their patients. Differences in clinical practice between physician specialties may have lasting consequences on patient health outcomes, though there is a dearth of real-world evidence available on the topic.
Objective: To describe treatment patterns and healthcare costs between PsA patients stratified by their treating provider’s specialty.
Methods: This study used administrative claims from the IBM® MarketScan® commercial and supplemental Medicare databases from 2014-2017. The sample included patients >18 newly diagnosed with PsA (first diagnosis=index date) with continuous plan enrollment for 12 months both preceding and following index date, an absence of infectious diseases, cancer, and any additional autoimmune disease excluding psoriasis, and an absence of any pharmacologic treatments indicated for PsA during the pre-index period. Patients treated with a medication for PsA were assigned to a physician specialty as observed during the 30-day period preceding the earliest medication claim. Patient not treated with PsA medications within the first 90 days after diagnosis were assigned to the provider listed on their diagnostic index claim. One-year outcomes included medication utilization including switching rates, and healthcare expenditures. Descriptive analyses were conducted by provider specialty and medication and included measures of central tendency and dispersion.
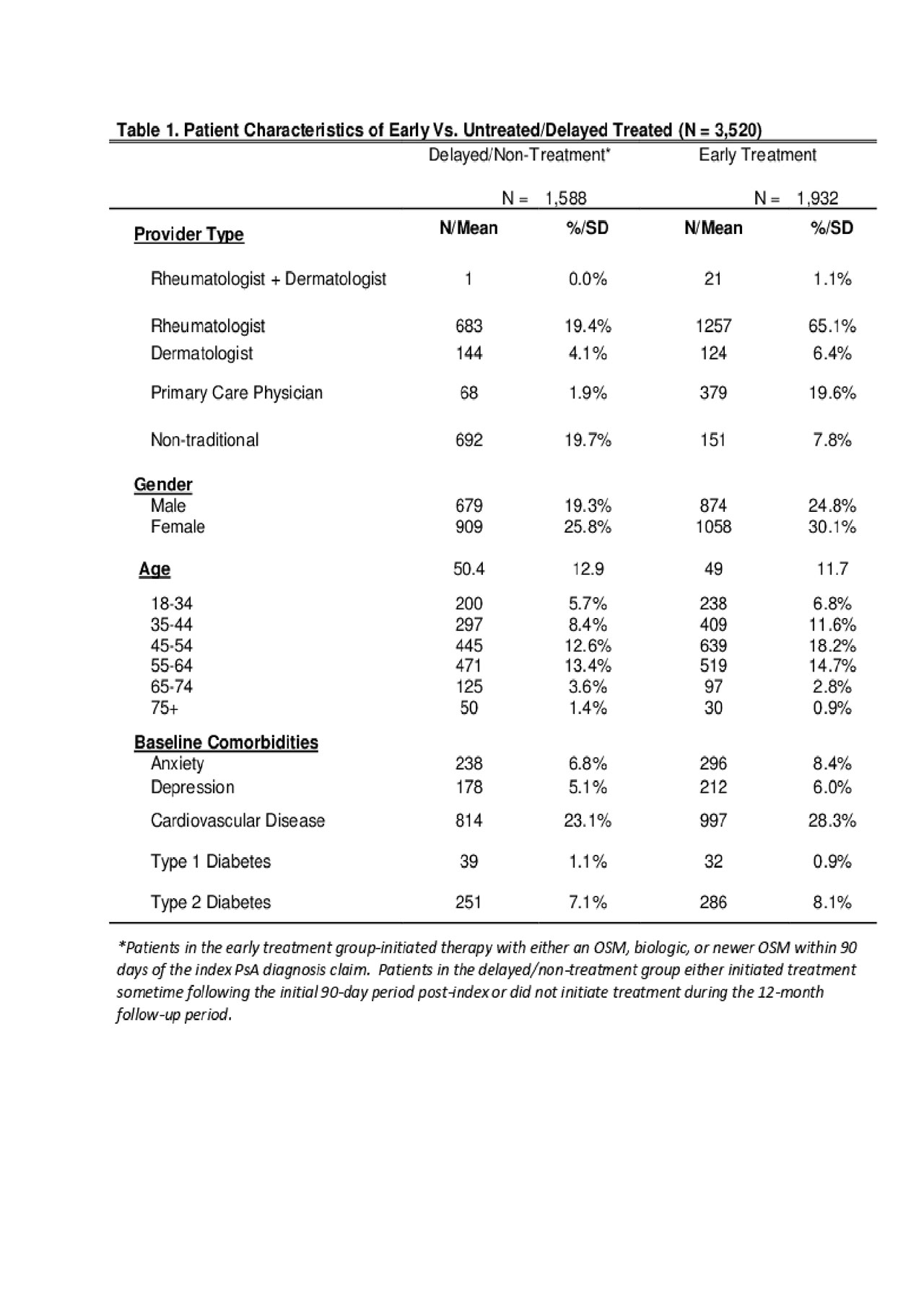
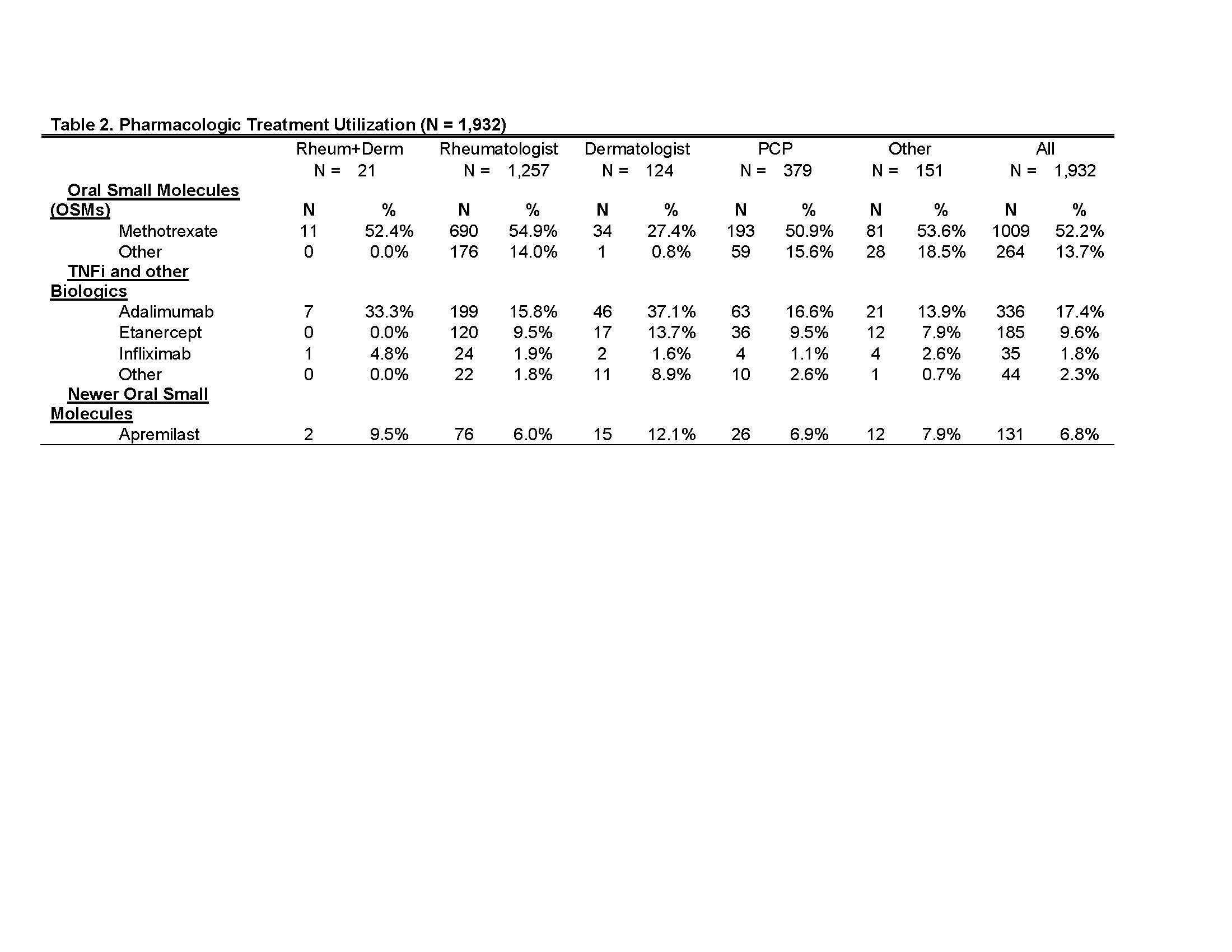
Results: 3,520 patients qualified for the study; the majority were female (56%) with an average age of 49.7. Of all rheumatologist’s PsA patients, about two thirds (65%) had early pharmacologic treatment, in contrast to approximately 46% of dermatologist’s patients (ps < 0.001). Of those with a medication, about 55% of these were prescribed by a rheumatologist; 8% by a dermatologist; < 1% by combination of both; 13% by a primary care provider (PCP); and 24% by others (e.g., pain management, physical medicine & rehab, etc.) (Table 1). Dermatologists were more likely to prescribe a TNFi (73%) compared to remaining provider groups (ranges 33%-48%; ps < 0.001) (Table 2). Mean total annual prescription and healthcare expenditures exhibited great variation for all provides, with rheumatologists and dermatologists having similar total costs despite lower prescription costs for rheumatologists (Figure 1).
Conclusion: There is significant variation in the pharmacologic treatment for PsA by different physician specialties. Our findings begin to uncover the impact of rheumatology practice patterns compared to other specialties. While more research is needed to confirm the findings, they highlight potential differences between rheumatologists and other physicians in managing costs and adherence to the recommended clinical guidelines for the management of PSA.
To cite this abstract in AMA style:
Tkacz J, Maksabedian E, Chan P, Limone B, Ogdie A, Karis E, Stolshek B. Describing Treatment Patterns and Healthcare Costs in Newly Diagnosed Psoriatic Arthritis Patients by Physician Specialty [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/describing-treatment-patterns-and-healthcare-costs-in-newly-diagnosed-psoriatic-arthritis-patients-by-physician-specialty/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/describing-treatment-patterns-and-healthcare-costs-in-newly-diagnosed-psoriatic-arthritis-patients-by-physician-specialty/