Session Information
Date: Sunday, November 10, 2019
Title: SLE – Animal Models Poster
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Lymphatic vessels are important in limiting the extent and duration of peripheral immune response, both by transporting cellular debris, inflammatory cells and excess interstitial fluid away from the site of inflammation, as well as through the direct modulation of the immune response by the lymphatic endothelial cells (LECs). Disruption in lymphatic function has been implicated in several models of chronic inflammatory diseases, including RA, psoriasis, and IBD. Cutaneous inflammation is a major feature of SLE, and is an important impediment to patients’ quality of life. The role of the lymphatic system in SLE, and its contribution to the cutaneous inflammatory phenotype of SLE specifically have not been described to date.
Methods: 7-10 weeks old (‘pre-diseased’) and 12 weeks old (‘diseased’) MRL/lpr (lpr) mice and age-/sex-matched MRL controls were evaluated at baseline, and after exposure to 2000-25000 J/m2 of ultraviolet radiation (UVR). Lymphatic function was assessed in 2 ways: 1) ‘Drainage’ – 1µL of 2% evans blue (EB) injected intradermally to the ear, followed by measurement of EB concentration in the draining lymph node (dLN) 1 minute later; or 2) ‘Effective clearance’ – evaluation of the residual dye concentration in the ear 18-24 hours following EB injection. EB concentration was evaluated by extraction of the dye from the tissue by immersion in formamide, followed by spectrophotometric evaluation of the fluid. Flow cytometry of the contralateral ears and dLNs was performed. Groups were compared with the Mann-Whitney U test; data is presented as median (interquartile range), with a two-tailed p-value of < 0.05 considered significant.
Results: Lymphatic clearance of EB from the ears of ‘diseased’ lpr mice was significantly impaired compared with controls (2.3-times residual EB in lpr ears at 24 hours post-EB injection, compared with controls, p=0.029). This difference in effective lymphatic clearance was not observed in ‘pre-diseased’ mice (0.85 (0.53-0.92) vs. 1 (0.79-1.21) in lpr vs. controls, p=0.8); indicating a possible association of dermal lymphatic dysfunction with disease activity (Figure 1). Similarly, when cutaneous inflammation was induced by UVR in ‘pre-diseased’ lpr and MRL mice, at 1 month-post UVR the lpr mice demonstrated significantly higher numbers of ear LECs than controls (1.42 (1.10-16.25) vs. 1 (0.95-1.05) of LECs per ear, normalized to MRL controls, p=0.009), but without the expected corresponding improvement in lymphatic drainage (0.92 (0.50-2.74) vs. 1 (0.57-1.43) EB in dLN, normalized to MRL controls, p=0.937); likely indicating a relative dysfunction in the lpr lymphatic vessel function.
Conclusion: The lymphatic network has long been known to be important in immune response regulation and tolerance mechanisms. SLE is thought to be the prototypical systemic inflammatory disease, but the role of the lymphatic system was never characterized in this setting. Here we provide evidence of impaired lymphatic function in the lpr lupus strain associated with increased disease activity, both due to age and UVR-induced inflammation. These findings may potentially point to a novel focus of study and intervention in this often devastating, yet still elusive disease.
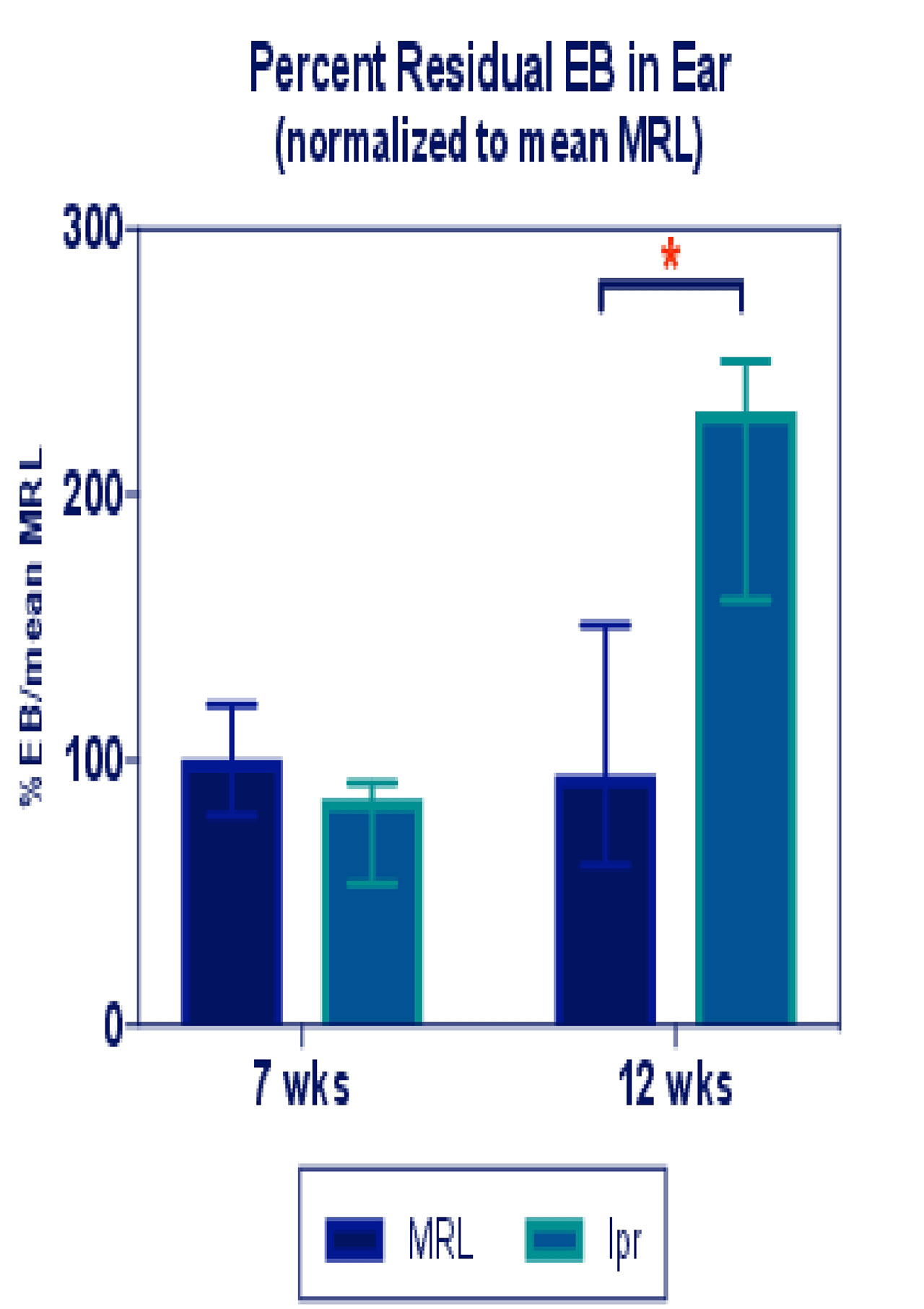
EB clearnace graph_ACR abstract
To cite this abstract in AMA style:
Schwartz N, Li T, Chyou S, Shipman W, Lu T. Dermal Lymphatic Dysfunction Is Associated with Disease Activity in the MRL/lpr Lupus Model [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/dermal-lymphatic-dysfunction-is-associated-with-disease-activity-in-the-mrl-lpr-lupus-model/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/dermal-lymphatic-dysfunction-is-associated-with-disease-activity-in-the-mrl-lpr-lupus-model/
