Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
Comorbidities
have an important impact on outcomes in chronic diseases. A new and simple to
compute index, the Rheumatic Disease Comorbidity Index (RDCI), has
recently been proposed in addition to existing indices. Evidence on its performance
in relation to functional status and health-related quality of life compared to
other known indices is scarce.
Medical
Dictionary for Regulatory Activities (MedDRA) is a
clinically validated international medical terminology dictionary used by regulatory
authorities and by researchers to code comorbidities and adverse events.
However, no simple algorithm is as yet available to convert MedDRA
classification into existing comorbidity indices.
Objective of
this study was o develop algorithms to calculate the
RDCI, Charlson-Deyo index (CDI) and Functional
comorbidity index (FCI) from MedDRA, and to test in
patients with RA how MedDRA-derived indices predict
function (HAQ) and health-related quality of life (based on SF-36).
Methods:
First, two
researchers coded the conditions listed in MedDRA
classification into the categories of each index. Next, using data from
patients with RA from the Norwegian NOR-DMARD study (2000-2012), we tested
predictive values of the RDCI, CDI, and FCI for physical function (HAQ) and
Physical and Mental Component Summary measures (PCS and MCS) from SF-36.
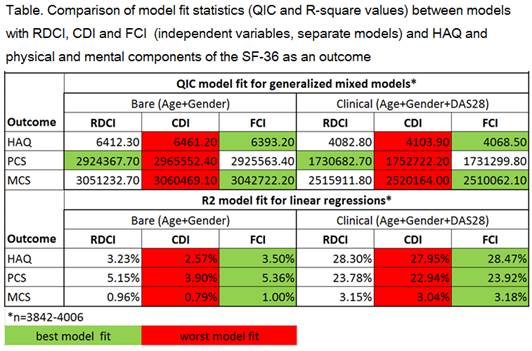
Outcomes (HAQ, MCS and PCS) were modeled at baseline and over time. Two models
were constructed for each outcome: a bare model (age and gender) and a clinical
model (including also DAS28). Generalised estimating
equations (GEE) (outcome over time) and linear regression models (outcome at
baseline) were fitted and model fit measures (the quasi likelihood under the
independence model criterion (QIC) for GEE and R-square for linear regression)
were compared. We examined which of the three indices provided the best model
fit to draw conclusions about the comparative performance of the indices: the
lower the QIC or the higher the R-square, the better the model fit.
Results:
Data from 4,080
patients were analysed (28.4% male, mean age 56 yrs, mean DAS28 at baseline 4.9). RDCI (mean 0.6, range
0-6) and FCI (mean 0.40, range 0-6) performed comparably well in predicting the
three outcomes considered. CDI (mean 0.24, range 0-7) performed worst on all
outcomes HAQ, SF-36 PCS and MCS. Of note, the comorbidities had almost no
influence on SF-36 MCS (Table).
Conclusion:
We have shown
that the MedDRA classification, which is widely used
in registries and clinical trials can be used to
compute currently used comorbidity indices. The new RDCI performed comparably
well with FCI on HAQ and the SF-36 (both physical and mental components). CDI
performed worst on all outcomes explored, but it needs to be reminded the CDI
was developed to predict mortality and not functioning.
To cite this abstract in AMA style:
Putrik P, Ramiro S, Lie E, Keszei A, Kvien TK, Uhlig T, Boonen A. Deriving a Comorbidity Index Form the Meddra Classification: Performance of Rheumatic Disease Comorbidity Index, Charlson-Deyo Index and Functional Comorbidity Index Among Patients with RA in NOR-DMARD Cohort [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/deriving-a-comorbidity-index-form-the-meddra-classification-performance-of-rheumatic-disease-comorbidity-index-charlson-deyo-index-and-functional-comorbidity-index-among-patients-with-ra-in-no/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/deriving-a-comorbidity-index-form-the-meddra-classification-performance-of-rheumatic-disease-comorbidity-index-charlson-deyo-index-and-functional-comorbidity-index-among-patients-with-ra-in-no/