Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The HPV vaccine is safe and immunogenic in RD patients but uptake is suboptimal. We aimed to evaluate factors associated with HPV vaccination in individuals with RDs, including RD diagnosis and age at diagnosis. We hypothesized that being diagnosed with an RD around the age when HPV vaccine initiation is recommended could pose a barrier to vaccination.
Methods: This retrospective study included individuals aged 16-22 seen by a rheumatologist in our academic center ≥2 times (2020-2022) who had an RD diagnosis and New York State (NYS) residence. We used chart review to ascertain demographics, immunization information (automatically pulled from the NYS Immunization Information System), RD diagnosis, and medications. We descriptively compared demographic and clinical variables between patients who had received 0-1 HPV vaccine doses (“unvaccinated”) and those who had received 2-3 doses (“vaccinated”) and performed multivariable logistic regression to assess the association between RD-related factors and HPV vaccination after adjusting for relevant demographic and clinical variables.
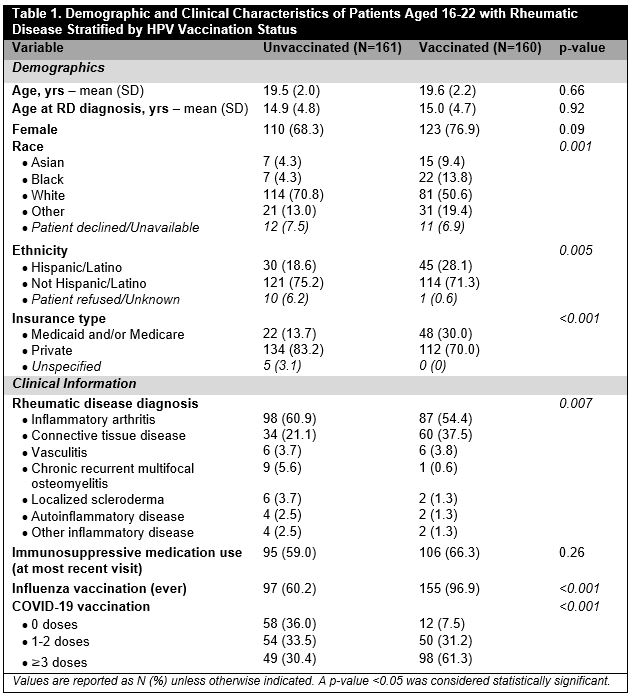
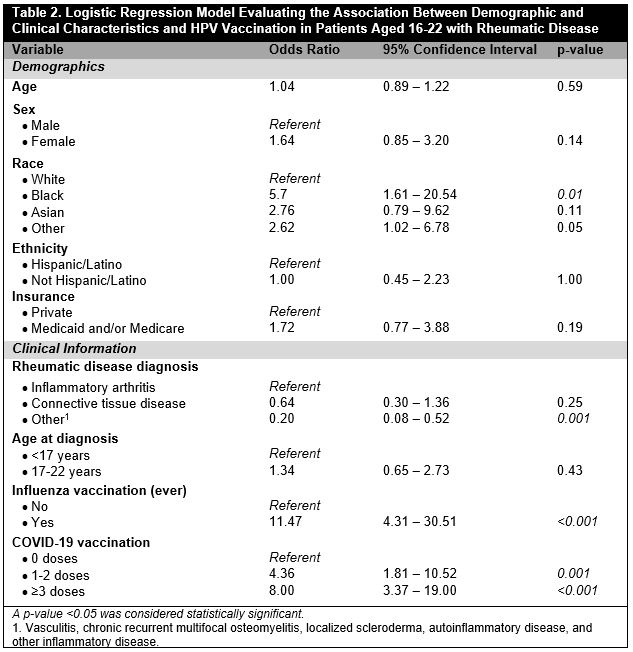
Results: Of 671 patients aged 16-22 seen by a rheumatologist ≥2 times in the study timeframe, 321 (47.8%) had an RD diagnosis and NYS residence. Mean age at most recent visit was 20 ± 2.1 years and at diagnosis was 14.9 ± 4.7 years, 233 (72.6%) were female, and 161 (50.2%) were unvaccinated. Compared to those who were vaccinated, unvaccinated individuals were more frequently White (70.8% vs 50.6%, p=0.001), non-Hispanic/Latino (75.2% vs. 71.3%, p=0.005), and privately insured (83.2% vs. 70.0%, p< 0.001). HPV vaccinated patients more frequently had received an influenza vaccine (96.9% vs. 60.2%, p< 0.001) or ≥3 COVID-19 vaccine doses (61.9% vs. 30.4%, p=0.003) compared to unvaccinated patients. RD diagnosis differed by HPV vaccine status (p=0.007): inflammatory arthritis (IA) was more common in unvaccinated vs. vaccinated patients (60.9% vs. 54.4%) and CTD was more common in vaccinated vs. unvaccinated patients (37.5% vs. 21.1%) [Table 1]. In multivariable analysis, Black vs. White patients with RD were more likely HPV vaccinated (OR 5.74, 95% CI [1.61-20.54], p=0.007) as well as those who had ever received an influenza vaccine vs. those who had not (OR 11.47, 95% CI [4.31-30-.51], p< 0.001); patients with “other” RD vs. IA were less likely HPV vaccinated (OR 0.20, 95% CI [0.08-0.52], p=0.001) [Table 2]. Age at RD diagnosis did not differ between groups and was not associated with HPV vaccination after adjustment.
Conclusion: In a large sample of patients aged 16-22 with RD, half had not received ≥2 HPV vaccine doses. As has been demonstrated in the general population, White race, non-Hispanic/Latino ethnicity, and having private insurance were associated with decreased HPV vaccine uptake. HPV vaccination was associated with influenza and COVID-19 vaccination, suggesting that some factors driving elective vaccine uptake are independent of vaccine type. Unvaccinated individuals more commonly had IA whereas vaccinated individuals more commonly had CTD; age at diagnosis was not associated with HPV vaccination after adjustment. Further research is needed to identify and mitigate barriers to HPV vaccination in this high-risk group.
To cite this abstract in AMA style:
Siegel C, Robinson L, Jannat-Khah D, Mikhaylov A, Pan N, Sammaritano L. Demographic and Clinical Factors Associated with HPV Vaccination in Young Adults with Rheumatic Disease [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/demographic-and-clinical-factors-associated-with-hpv-vaccination-in-young-adults-with-rheumatic-disease/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/demographic-and-clinical-factors-associated-with-hpv-vaccination-in-young-adults-with-rheumatic-disease/