Session Information
Date: Friday, November 6, 2020
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Psoriatic arthritis (PsA) is a heterogeneous disease which may precede, occur concurrently or after the development of psoriasis. In order to better understand the natural history of the disease we aimed to identify demographic and clinical characteristics associated with delay in transition from psoriasis to PsA.
Methods: A retrospective, population-based cohort of incident PsA patients ≥18 years of age from a geographically-defined area meeting ClASsification of Psoriatic ARthritis (CASPAR) criteria for PsA (2000-17) was identified. Onset of psoriasis was defined as confirmatory diagnosis of psoriasis by a dermatologist or rheumatologist. Date of fulfillment of CASPAR criteria was considered as the time of onset of PsA. PsA patients were divided into two groups: patients with concurrent psoriasis and PsA (within one year of each other) and patients with psoriasis onset before PsA ( >1 year). Those patients with psoriasis development after PsA onset ( >1 year) or only family history of psoriasis were excluded. Logistic regression models adjusted for age and sex were performed to identify factors associated with delay in transition from psoriasis to PsA.
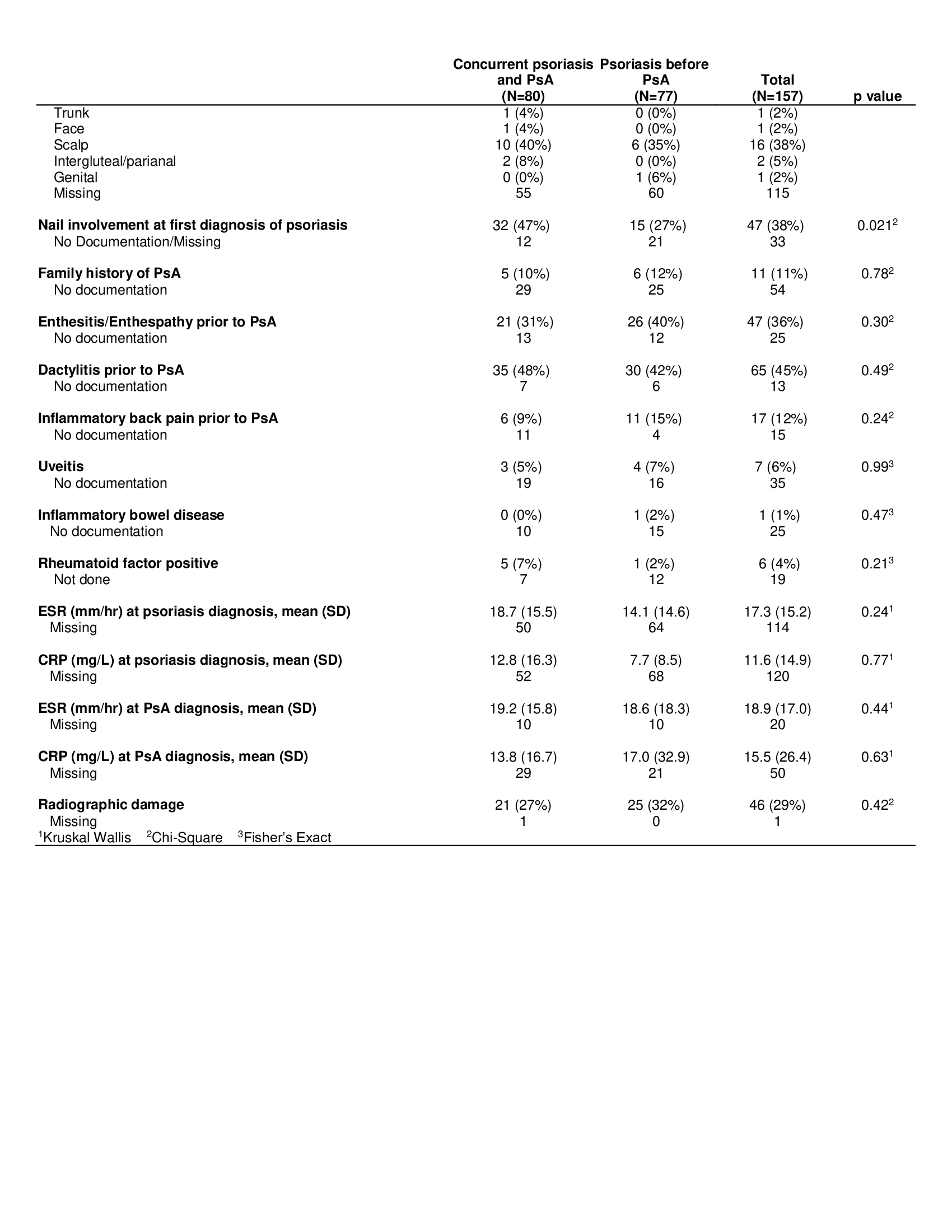
Results: There were 157 incident cases of PsA, mean age at diagnosis was 46.3 (SD=12.0) years and 46% were females. Median lag time from psoriasis onset to PsA was 263 days (interquartile range=0, 2889). 51% (n=80) of patients had concurrent psoriasis and PsA while 49% (n=77) had onset of psoriasis before PsA (Table 1). Family history of psoriasis (OR= 2.71, 95% CI 1.24 – 5.90) and psoriasis severity (OR=1.96, 95% CI 1.26 -3.06) were more likely in those who had a delay in transition from psoriasis to PsA than those who had a concomitant diagnosis (Table 2). There were no statistically significant differences in demographic features, or any of the other psoriasis or PsA related factors between the 2 groups. Similarly, no difference in radiographic outcome was noted for the 2 groups.
Conclusion: In this population-based study, approximately half of the patients had psoriasis onset before PsA, and the other half had concurrent psoriasis and PsA. Patients with a family history of psoriasis and severe psoriasis were more likely to have a delay in transition from psoriasis to PsA. Whether this difference is secondary to earlier detection of psoriasis in patients with a family history of psoriasis and severe psoriasis or a true phenotypic difference will require further studies.
 Table 1. Baseline characteristics of patients with concurrent psoriasis and PsA, and psoriasis before PsA
Table 1. Baseline characteristics of patients with concurrent psoriasis and PsA, and psoriasis before PsA
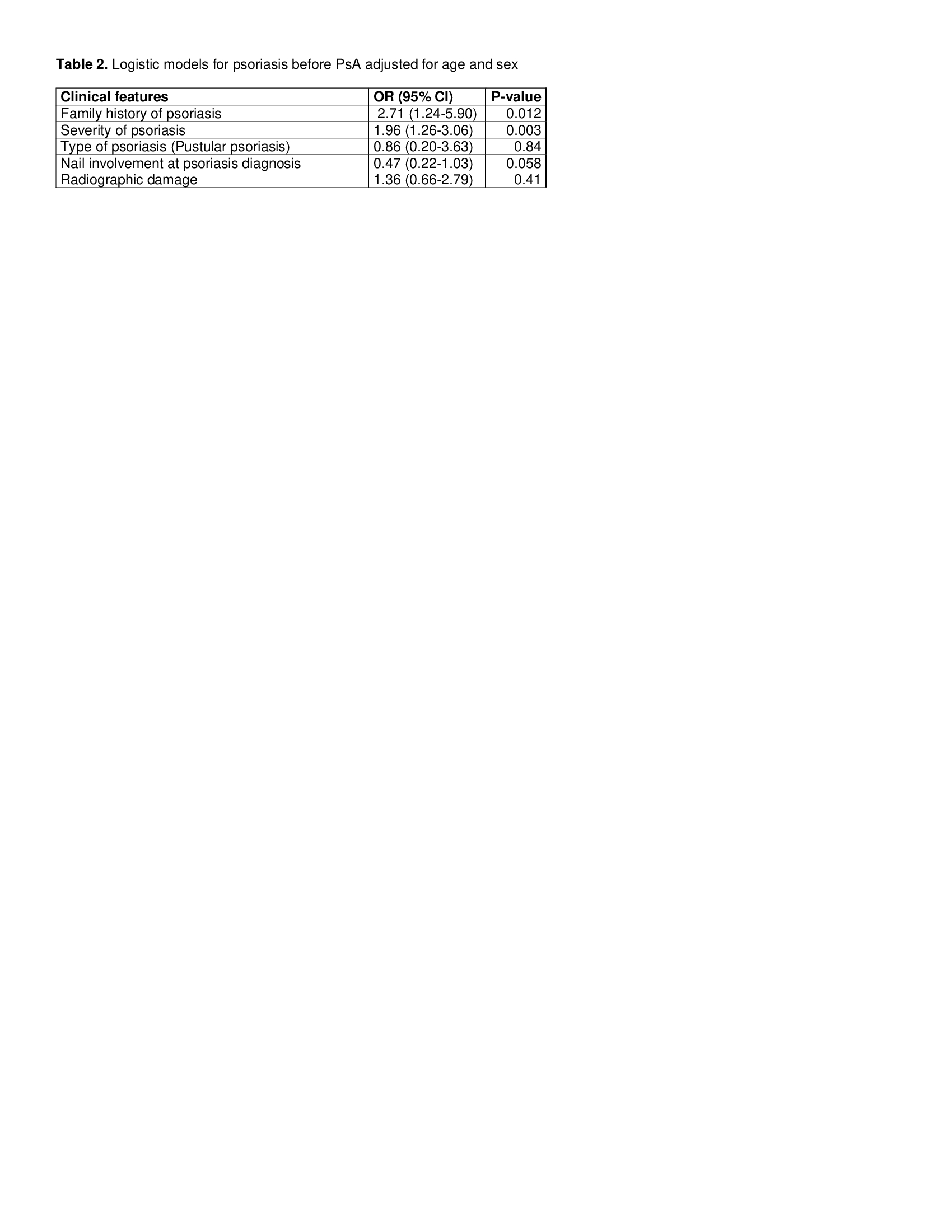 Table 2. Logistic regression models for psoriasis before PsA adjusted for age and sex
Table 2. Logistic regression models for psoriasis before PsA adjusted for age and sex
To cite this abstract in AMA style:
Karmacharya P, Wright K, Achenbach S, Bekele D, Crowson C, Ogdie A, Duarte-Garcia A, Ernste F, Tollefson M, Davis J. Delay in Transition from Psoriasis to Psoriatic Arthritis: A Population Based Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/delay-in-transition-from-psoriasis-to-psoriatic-arthritis-a-population-based-study/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/delay-in-transition-from-psoriasis-to-psoriatic-arthritis-a-population-based-study/