Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose
MRI is a sensitive method to detect early signs of axial spondyloarthritis (axSpA). A positive MRI of the sacroiliac joints is part of the imaging arm of the ASAS criteria. However, the exact role of MRI of the spine in screening for axSpA needs to be determined. Degenerative changes (DCs) are a common finding in the spine of adults; they might be an alternative explanation for complaints and might interfere with diagnostic decision making. Purpose of this study was to describe the prevalence of DCs on spine MRI in axSpA and no axSpA patients in the DESIR cohort
Methods
The DESIR cohort is a prospective longitudinal cohort study of adults aged 18-50 with inflammatory back pain (IBP) ≥3 months, ≤3 years. Patients (pts) were categorized as axSpA or no axSpA, based on the ASAS criteria for axial spondyloarthritis. Baseline 1.5T MRI (sagittal T1TSE and STIR) of the spine were scored independently by two blinded readers, for: degree of disc degeneration (DD) (Pfirrmann 5 point scale, class ≤2 considered normal), endplate changes (Modic 3 point scale) and presence of a high intensity zone (HIZ), disc protrusion or extrusion, canal stenosis, spondylolisthesis, facet joint osteoarthritis (FJOA) and Schmorls nodes (±edema). In case of disagreement, a third reader acted as adjudicator. AxSpA and no axSpA pts were compared using chi2 test, regression analysis was used for association between age and DCs
Results
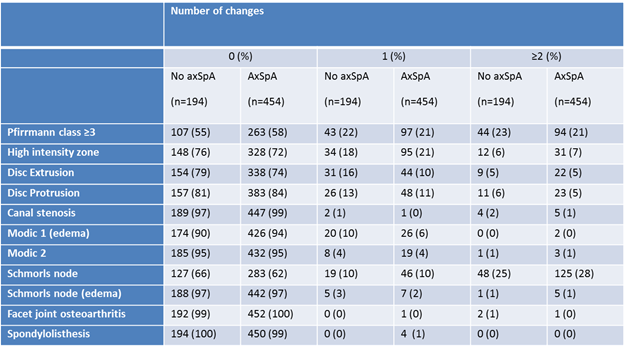
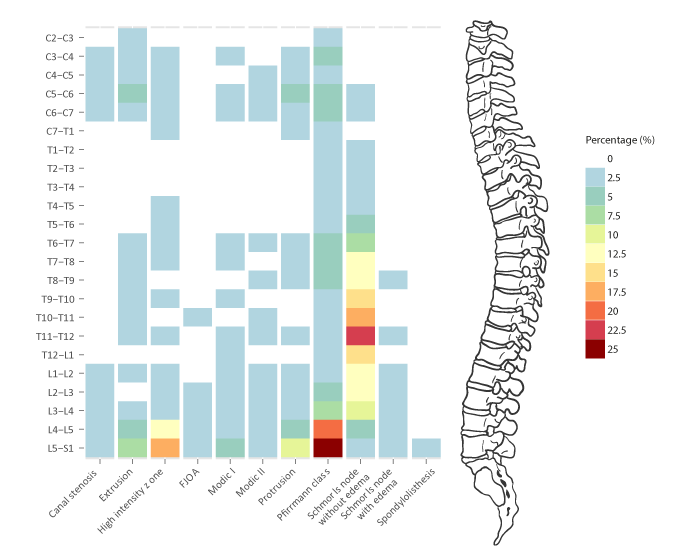
648 pts (303 male, 47%) with mean age 34 (±9) had a MRI spine available and were evaluated. Of these, 454 (70%) had axSpA. 456 pts (70%) showed one or more DCs (range 1-39). In 366 (57%) pts, DCs were observed in the lumbar spine and in 292 (45%) pts in L4-S1 (fig 1). Less pts had DCs in the cervical spine (119, 18%), and thoracic spine (253, 39%). DD and Schmorls nodes were most prevalent (table 1, fig 1). Modic type 3 was not observed. Table 1 lists the number of pts with none, one or multiple changes.
192(30%) pts with no DCs were evenly distributed between the axSpA and no axSpA groups (56/194, 29% and 136/456, 30%) (P=.854). With increasing age, the total number of DCs increased (b=0.11; P<.001) and this was also for canal stenosis, extrusion, HIZ, FJOA, Modic I and Pfirrmann (b=.002 to .058; P=.047 to <.001).
Conclusion
Prevalence of DCs is high in pts with IBP in the DESIR cohort and in accordance with literature. Most DCs are found in the (lower) lumbar spine. With age, the prevalence of DCs increased. No difference was found between axSpA and no axSpA pts.
Table 1
Figure 1: The prevalence of all degenerative changes for each vertebral unit is shown on this heatmap. The darker the colour, the higher its prevalence (as indicated in the colour key on the right).
Disclosure:
F. de Bruin,
None;
M. O. Treyvaud,
None;
A. Feydy,
None;
M. Dougados,
None;
L. Gossec,
None;
J. L. Bloem,
None;
D. van der Heijde,
None;
M. Reijnierse,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/degenerative-changes-of-the-spine-on-mri-in-patients-with-inflammatory-back-pain-from-the-desir-cohort/