Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Sarcoidosis has been suggested to occur with connective tissue diseases (CTDs) more frequently than would be expected by chance, but the types, relative timing, and prognosis of the associated CTDs are not well-described. The objective of this study is to define relative timing of sarcoidosis with CTD to determine whether one could predispose to another. Our secondary objectives are patient demographics, medication triggers, antibody profiles and frequency of overlap with each CTD. We analyzed a large institutional retrospective cohort of patients with overlapping CTD and sarcoidosis, to identify and explore these features.
Methods: For this descriptive study using retrospective chart review we identified patients with a dual diagnosis of sarcoidosis and one of 6 other CTDs (RA, SLE, inflammatory myositis, SpA, SSc or Ss) seen within the Division of Rheumatology from October 2015 to October 2017 in our health system, using ICD-10 codes. These were manually validated by chart review. If patients did not have a diagnosis of CTD and/or sarcoidosis confirmed by Rheumatology or lacked data to validate both of these diagnoses by ACR classification, they were excluded.
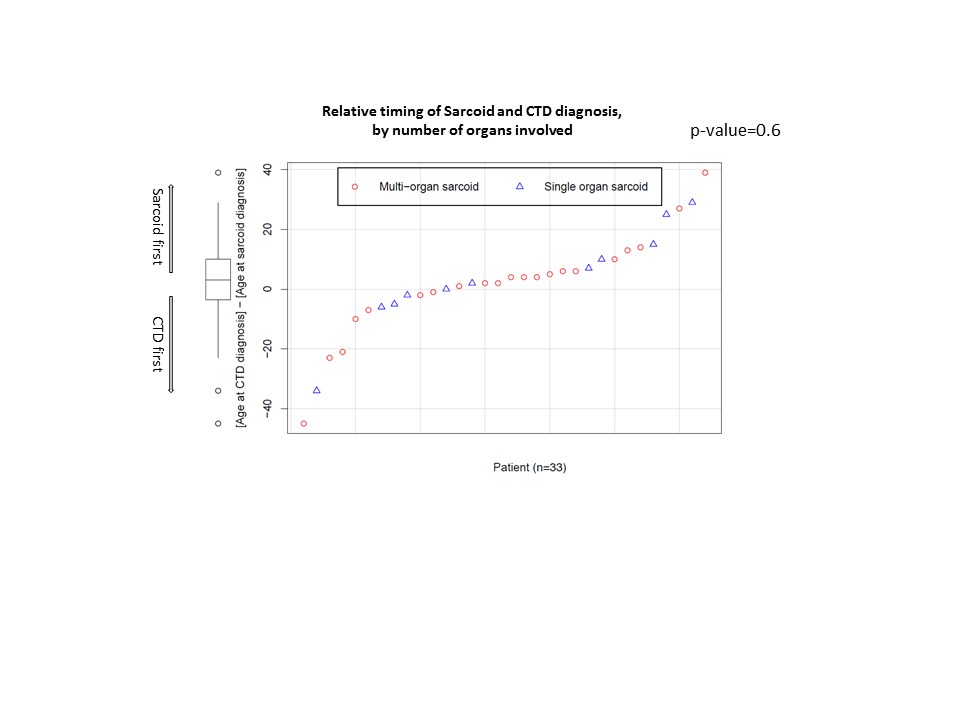
Results: 66 charts matched our query and on individual review, 33 patients fulfilled our criteria. 70% of our patients were female and 64% were black. Mean age at diagnosis of CTD was 46 (SD16.4) years and of sarcoidosis was 44 (14.4) years. There was no predisposition towards development of sarcoidosis or CTD first (p=0.6). 58% (19) of patients had RA, 15% (5) had SLE, 15% (5) SSc, 9% (3) SpA, and 3% (1) myositis. 12% (4) of patients had secondary Ss. Lung was the most common organ involved with sarcoidosis (88%); 58% of patients had Scadding stage I disease, and only 1 (3%) had stage IV disease. The odds of single organ sarcoidosis were not different whether the CTD or sarcoidosis was diagnosed first (p=0.7); the order of diagnosis did not predict sarcoidosis remission (p=0.3). There was a high prevalence of positive ANA throughout the cohort (73% of the 24 with available data). Of 29 patients with data, RF was present in 9 (45%) patients with RA, versus 1 (11%) of patients without RA (p=0.1). TNF-alpha inhibitor induced sarcoidosis developed in two patients with RA and one with SpA.
Conclusion: The timing of CTD and sarcoidosis development in this cohort does not argue for a strong effect of CTD predisposing to sarcoidosis or vice versa, and the clinical course of sarcoidosis is similar whether diagnosed before or after the CTD. RA was most commonly associated with sarcoidosis. A High prevalence of Scadding Stage I disease may point to a close link of sarcoidosis with inflammatory disease, as does a high prevalence of ANA and RF across the cohort. Further information from a case control study is needed to draw generalizable conclusions.
To cite this abstract in AMA style:
Agrawal M, Ligon C. Defining Characteristics of Patients with Overlap between Sarcoidosis and Connective Tissue Diseases [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/defining-characteristics-of-patients-with-overlap-between-sarcoidosis-and-connective-tissue-diseases/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/defining-characteristics-of-patients-with-overlap-between-sarcoidosis-and-connective-tissue-diseases/