Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose: Despite the lack of evidence to support the use of opioids in the treatment of adult fibromyalgia syndrome, approximately 30% of patients receive an opioid prescription (Fitzcharles, Am J Med. 2011). The prevalence of and risk factors for opioid prescribing for juvenile fibromyalgia syndrome (JFMS), however, have not been established.
Methods: We performed a retrospective cohort study using de-identified healthcare claims data from ClinformaticsTM DataMart (OptumInsight, Eden Prairie, MN) from May 2000 – June 2013. The index date was the first ICD-9 code for fibromyalgia (729.1). JFMS was defined as subjects ≥ 2 and < 18 years of age at the index date with ≥2 codes for fibromyalgia within 12 months and continuous enrollment 6 months prior to and 12 months after the index date. Subjects with burns, sickle cell disease, or malignancy were excluded. Opioid exposure was defined as ≥ 1 prescription within 6 months prior to or any time after the index date. Healthcare utilization was assessed by provider type and place of service and defined as ≥ 1 co-variate prior to first opioid prescription. Acute care visit included an urgent care and/or emergency department encounter. Multivariate logistic regression modeling (adjusting for demographics, co-morbidities, and healthcare utilization) was used to identify independent risk factors associated with opioid use.
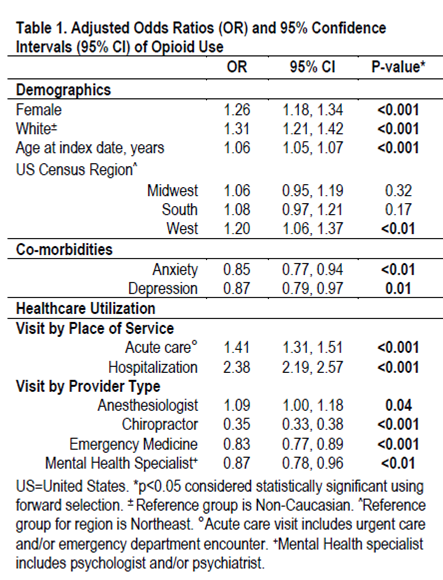
Results: Of 26516 subjects who met study criteria, 5296 (20%) received an opioid prescription. Subjects were predominantly female (55%) and Caucasian (80%). Median age at index date was 14 years (IQR: 11.0, 16.0) and at first opioid prescription was 16 years (IQR: 13, 17). Codeine (71%), tramadol (21%) and oxycodone (14%) were the most commonly prescribed opioids. Diagnosis of anxiety and depression occurred in 14% and 15% of children, respectively. In multivariate logistic regression (Table 1), opioid exposure was positively associated with female sex (OR =1.26; p<0.001), Caucasian race (OR=1.31; p<0.001), preceding acute care visit (OR: 1.41; p<0.001), hospitalization (OR: 2.38; p<0.001) and anesthesiology encounters (OR: 1.09; p=0.04). Compared to the Northeast, subjects from the Western United States had an increased risk of opioid exposure (OR: 1.20; p<0.01). Presence of a mental health co-morbidity and an encounter with a mental health provider were associated with decreased risk of opioid use (all p<0.05). Children seen by a chiropractor or emergency medicine physician also had a decreased risk of opioid use (OR: 0.35 and OR: 0.83, respectively; both p<0.001).
Conclusion: Opioids were prescribed for 20% of children with JFMS. Increased physician education in acute care and inpatient settings is needed to reduce prescribing of opioids for JFMS. Increased availability of mental health resources and non-pharmacologic treatment options might represent effective strategies to reduce opioid exposure in children with JFMS.
To cite this abstract in AMA style:
Gmuca S, Xiao R, Knight AM, Sherry DD, Weiss PF, Gerber JS. Curbing the Opioid Epidemic: Predictors of Opioid Use in Juvenile Fibromyalgia Syndrome [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/curbing-the-opioid-epidemic-predictors-of-opioid-use-in-juvenile-fibromyalgia-syndrome/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/curbing-the-opioid-epidemic-predictors-of-opioid-use-in-juvenile-fibromyalgia-syndrome/