Session Information
Date: Monday, November 8, 2021
Title: Epidemiology & Public Health Poster III: Other Rheumatic & Musculoskeletal Diseases (1022–1060)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Patients with systemic rheumatic diseases (SRD) have an increased risk of admission to the Intensive Care Unit (ICU) relative to the general population, secondary to SRD chronicity, expanding options for concomitant immunosuppression, co-morbidities, deconditioning, and multi-organ disease. Despite this, there is paucity of data within this population regarding outcomes of ICU admission over time, and whether subgroups of patients with SRD exhibit differential outcomes. This study aims to further the understanding of SRD in the context of critical illness by examining a population-based registry, the Australia New Zealand Intensive Care Society Adult Patient Database (ANZICS-APD).
Methods: The ANZICS-APD mandates disease-category based reporting across all ICUs in ANZ, including mortality and length of stay both within ICU and hospital. Retrospective data (2004-2019) from ICU admissions across hospitals in Australia and New Zealand was analysed. Eligible records were those where the primary reason for admission was SRD. These were identified through the use of database specific codes and excluded sepsis, rhabdomyolysis and viral myositis. We sought to analyse the trends over time, mortality and length of stay across SRDs. Severity of critical illness on ICU admission was measured by the Australian and New Zealand Risk of Death (ANZROD) score.
Results: 1,478 admission episodes (52% females) were included, from 155 Australian sites (95%) and 16 New Zealand sites (5%). Reasons for admission were musculoskeletal/skin (42%), musculoskeletal medical (38%), vasculitis (7%), connective tissue disease (5%), SLE (3%), scleroderma (2%) and rheumatoid arthritis (RA; < 2%). Predicted mortalities for each diagnosis (derived from the ANZROD scoring system) were: connective tissue disease 17%, vasculitis 17%, SLE 15%, musculoskeletal-medical 10%, scleroderma 10%, musculoskeletal-skin disease 9.3% and RA 5.2%. Considering temporal changes, annual ICU admissions with SRD increased in a linear fashion from 2004 to 2019, consistent with growth in the size of the database over time. Change in hospital mortality over time was not statistically significant and remained stable or decreased over this period (Figure 1). Median length of hospital stay did not demonstrate a temporal trend (Figure 2). In-hospital mortality by SRD category was connective tissue disease (17%), vasculitis (10%), SLE (9%), musculoskeletal-medical (9%), scleroderma (20%), musculoskeletal/skin (7%) and RA (4%).
Conclusion: Analysis of a large dataset from Australian and New Zealand ICUs reveals that: 1) There has been a large increase in the number of patients with SRD admitted to ICUs each year since 2004, a change reflected in the ANZICS-APD more broadly 2) In-hospital mortality in this cohort remained stable or decreased over time; 3) No temporal trend with respect to length of ICU stay is apparent; 4) Patients with connective tissue disease, vasculitis and SLE are sicker on presentation relative to other SRD diagnoses; and 5) In-hospital mortality is greatest in patients with scleroderma or connective tissue disease.
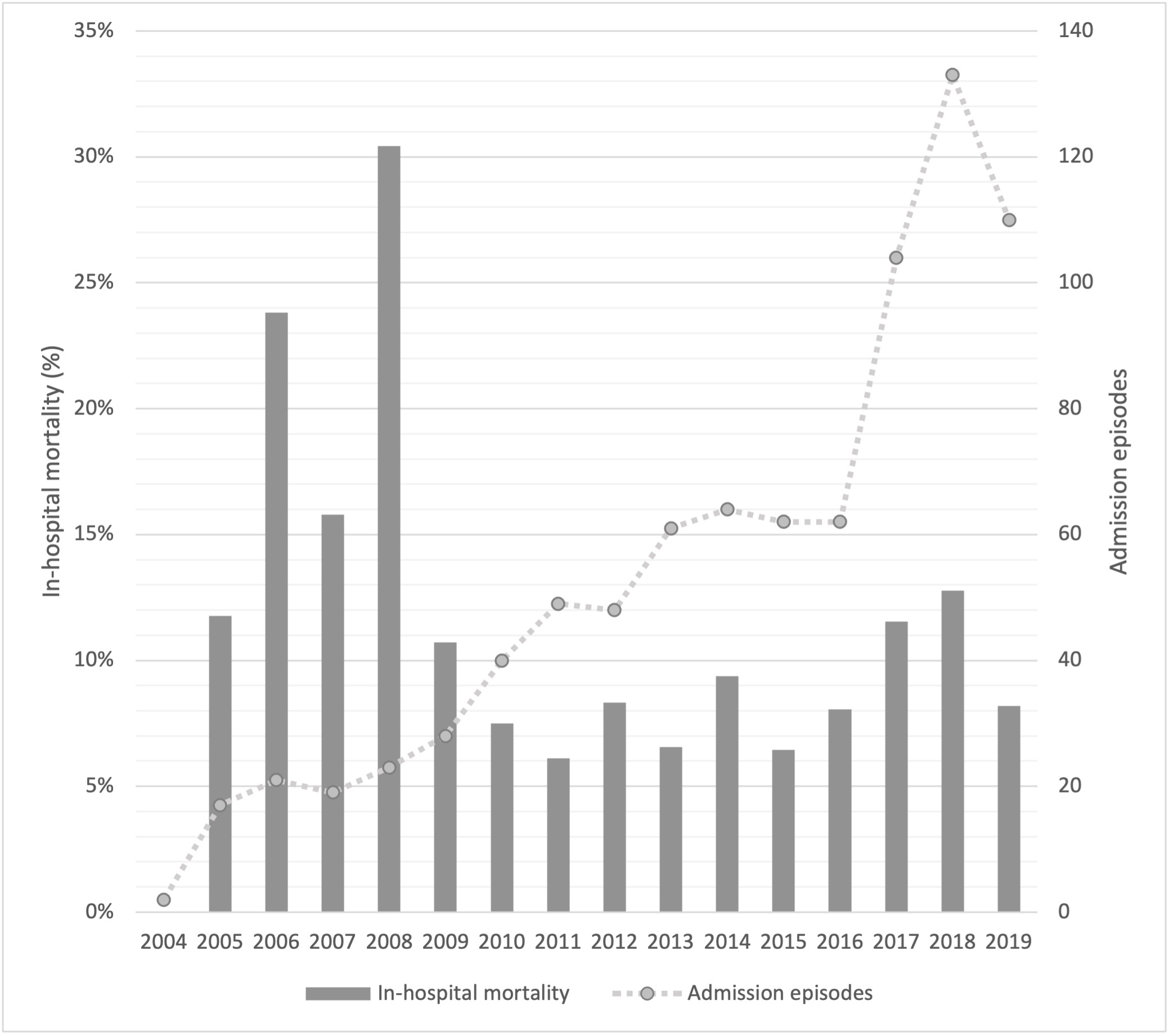 Figure 1 Admission episodes and in-hospital mortality over time
Figure 1 Admission episodes and in-hospital mortality over time
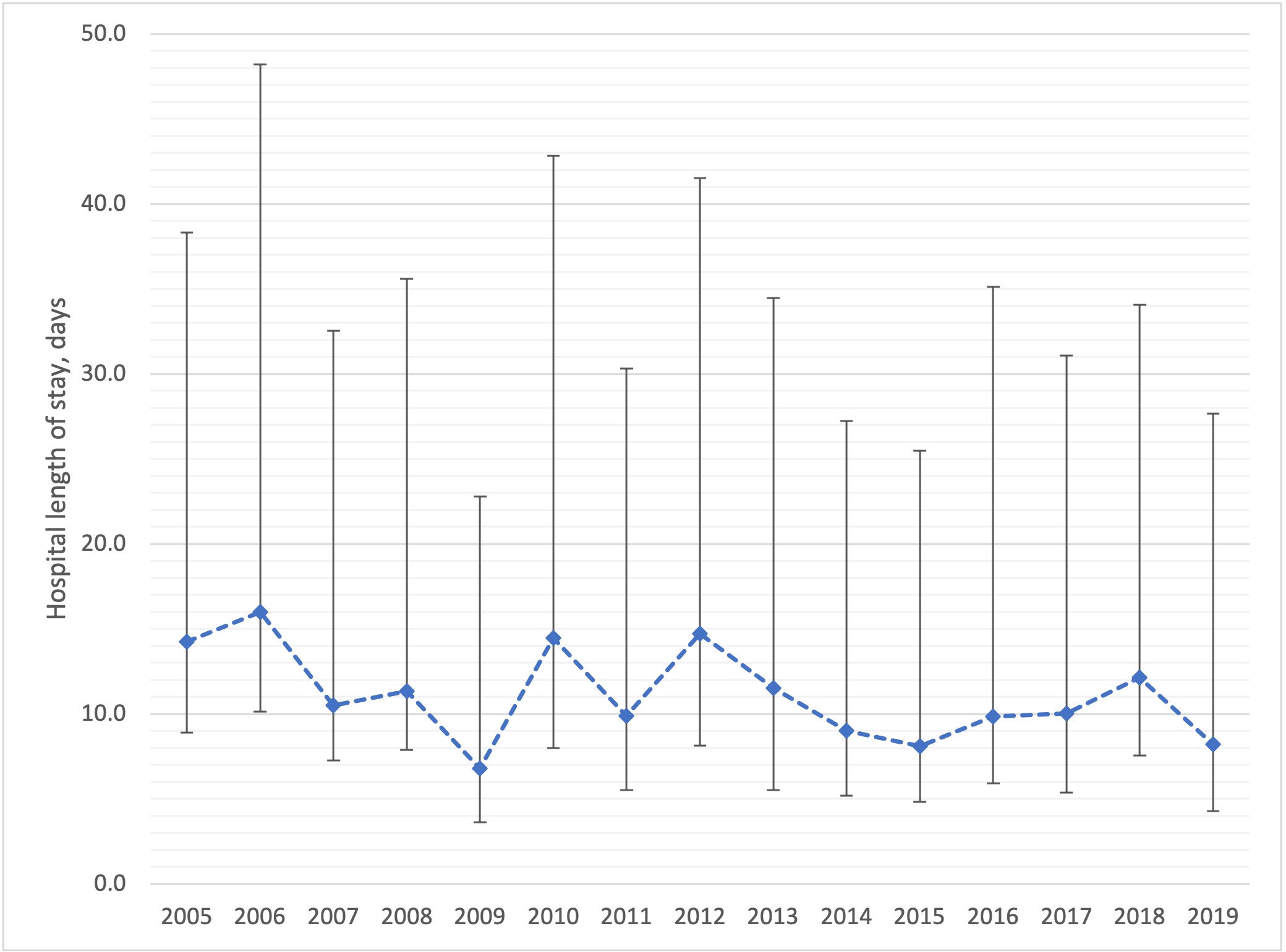 Figure 2 Median (IQR) length of hospital stay by year
Figure 2 Median (IQR) length of hospital stay by year
To cite this abstract in AMA style:
Lambert R, Bihari S, Wechalekar M, Pilcher D, Pontifex E. Critical Illness in Modern Rheumatology: Analysis of Admissions to Australian and New Zealand ICUs [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/critical-illness-in-modern-rheumatology-analysis-of-admissions-to-australian-and-new-zealand-icus/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/critical-illness-in-modern-rheumatology-analysis-of-admissions-to-australian-and-new-zealand-icus/
