Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: COVID-19 vaccine uptake in autoimmune and inflammatory rheumatic disease (AIIRD) patients is an area of concern to rheumatologists and other providers. These patients are at a greater risk of infection and COVID-19-related complications due to underlying conditions and therapies. The purpose was to ascertain COVID-19 vaccine and booster uptake, reasons for hesitancy, and self-reported flare in a large rheumatology practice-based network (PBRN).
Methods: A tablet-based survey was deployed as part of routine care in 104 rheumatology practices who were members of the Excellence Network in RheumatoloGY (ENRGY) PBRN during 12/2021- 12/2022. Patients were asked about COVID-19 vaccine status and why they might not receive a vaccine or booster. Patients reporting no vaccine receipt were asked additional questions about why they did not receive the vaccine and were categorized as vaccine-hesitant. Receipt of the primary series of vaccines and a response of “not planning to” or “not sure ”when asked about getting additional vaccine or booster doses defined booster-hesitant patients. We used descriptive statistics to explore the differences between vaccination status and vaccine/booster hesitancy, comparing AIIRD to non-AIIRD patients. We used multivariable logistic regression to estimate adjusted odds ratios (aOR) with confidence intervals (CI), examining the association between vaccine uptake and AIIRD status, and self-reported flare/disease worsening and AIIRD status.
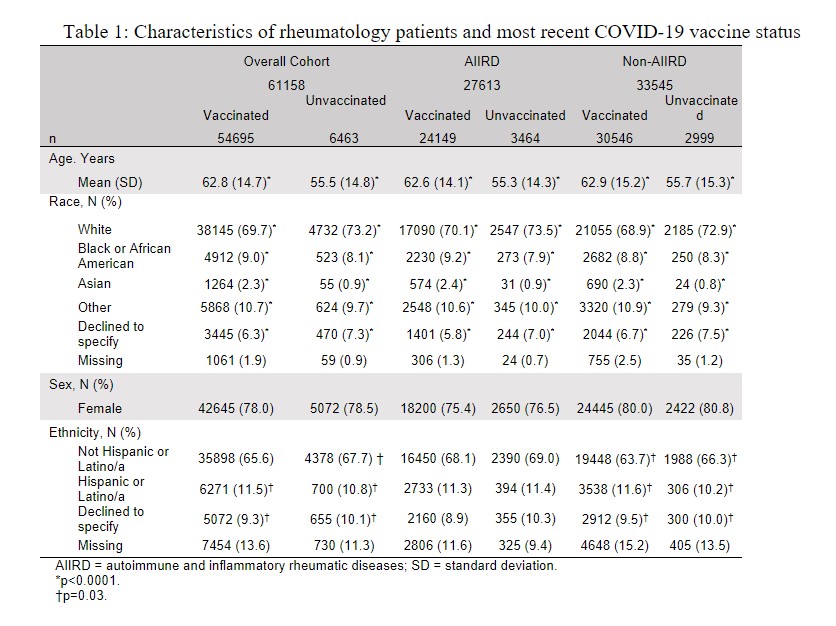
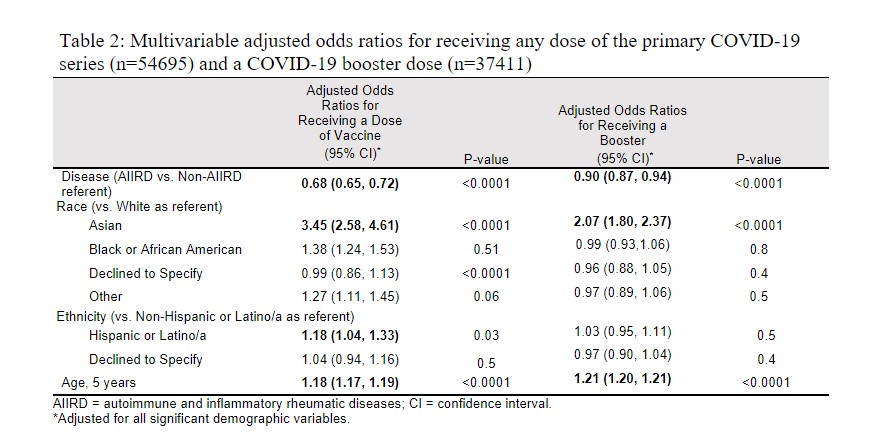
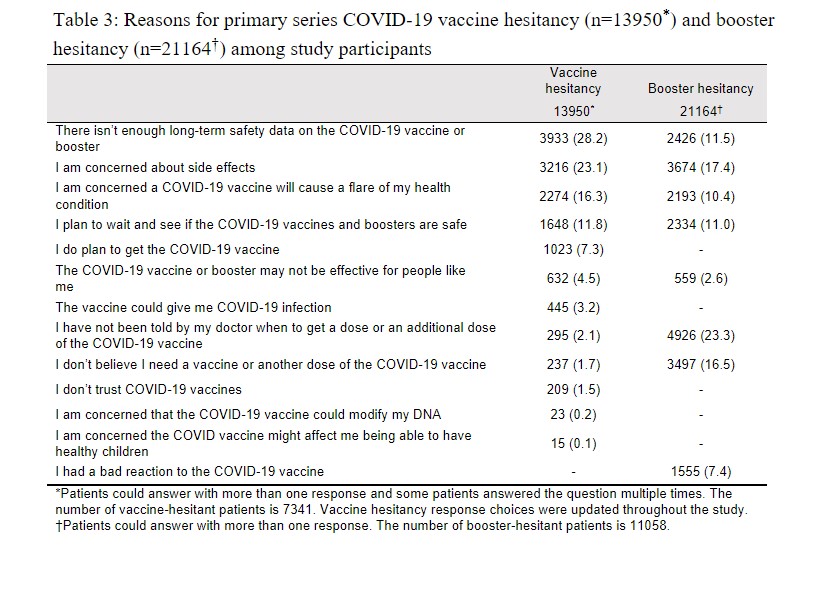
Results: Of 61,158 respondents (99.9% completion rate), 89% reported at least one dose of vaccine; of the vaccinated, 68% reported at least one booster (Table 1). AIIRD patients were 32% less likely to receive a vaccine (aOR: 0.68; 95% CI: 0.65, 0.72) and 10% less likely to receive a booster (aOR: 0.90; 95% CI: 0.87, 0.94) versus non-AIIRD patients (Table 2). A greater proportion of AIIRD patients were vaccine-hesitant (14% vs. 10%; p< 0.0001) and booster-hesitant (21% vs. 16%; p< 0.0001) compared to non-AIIRD patients. Among those who were vaccine hesitant (n=7,341), safety concerns (28%) and side effects (23%) were the main reasons for vaccine hesitancy, while among those who were booster hesitant (n=11,058), lack of recommendation from the physician was the primary factor for booster hesitancy (23%) (Table 3). Of those who received a vaccination, 23% of patients reported experiencing symptoms consistent with reactogenicity or a flare/disease worsening following their most recent vaccination. AIIRD patients did not have increased odds of self-reported flare/worsening disease compared to non-AIIRD patients (aOR: 0.99; 95% CI: 0.94, 1.05). Among the vaccine-hesitant and booster-hesitant, 12% and 39% later reported receiving a respective dose.
Conclusion: A meaningful proportion of vaccine- and booster-hesitant patients eventually received vaccination or booster doses, suggesting that future interventions tailored to AIIRD patients to encourage vaccination or booster use may be fruitful.
To cite this abstract in AMA style:
Holladay E, Mudano A, Xie F, Stewart P, Jackson L, Danila M, Gavigan K, Nowell W, Venkatachalam S, Curtis J. COVID-19 Vaccine Uptake, Hesitancy, and Flare in a Large Rheumatology Practice Network [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/covid-19-vaccine-uptake-hesitancy-and-flare-in-a-large-rheumatology-practice-network/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/covid-19-vaccine-uptake-hesitancy-and-flare-in-a-large-rheumatology-practice-network/