Session Information
Date: Saturday, November 6, 2021
Title: Epidemiology & Public Health Poster I: COVID-19 & Vaccination (0084–0117)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Following SARS-CoV-2 infection, patients with rheumatic diseases seem to have similar or slightly poorer outcomes compared with those without rheumatic disease. However, robust data is lacking to inform our understanding of mortality and morbidity following COVID-19 infection in patients with rheumatic diseases.
Methods: The University of Utah COVID-19 database identifies all adult patients that tested positive with Covid-19 at a University of Utah facility throughout the state of Utah. This database was used to identify and glean data from all Covid-19 positive patients retrospectively from January 1, 2020 to March 26, 2021. Patients with rheumatic diseases testing positive for Covid-19 were identified from this database using ICD-10 codes of the most common rheumatic diseases, including rheumatoid arthritis, lupus, inflammatory myositis, vasculitis, spondyloarthritis, sarcoidosis, and gout. Outcomes of interest included mortality, hospitalization, and length of stay. For each outcome, we conducted univariable analysis and used weighted (propensity scores) and unweighted multivariable logistic regression to estimate odds ratio (ORs) and 95% confidence interval (CI) based on the presence of rheumatic diseases. Age, sex, Charleson Comorbidity Index (CCI) and BMI were included as covariates in multivariable logistic regression models. Subgroup analysis was performed for glucocorticoids, conventional synthetic disease modifying agents (cDMARDs) and biological disease modifying agents (bDMARDs) medications.
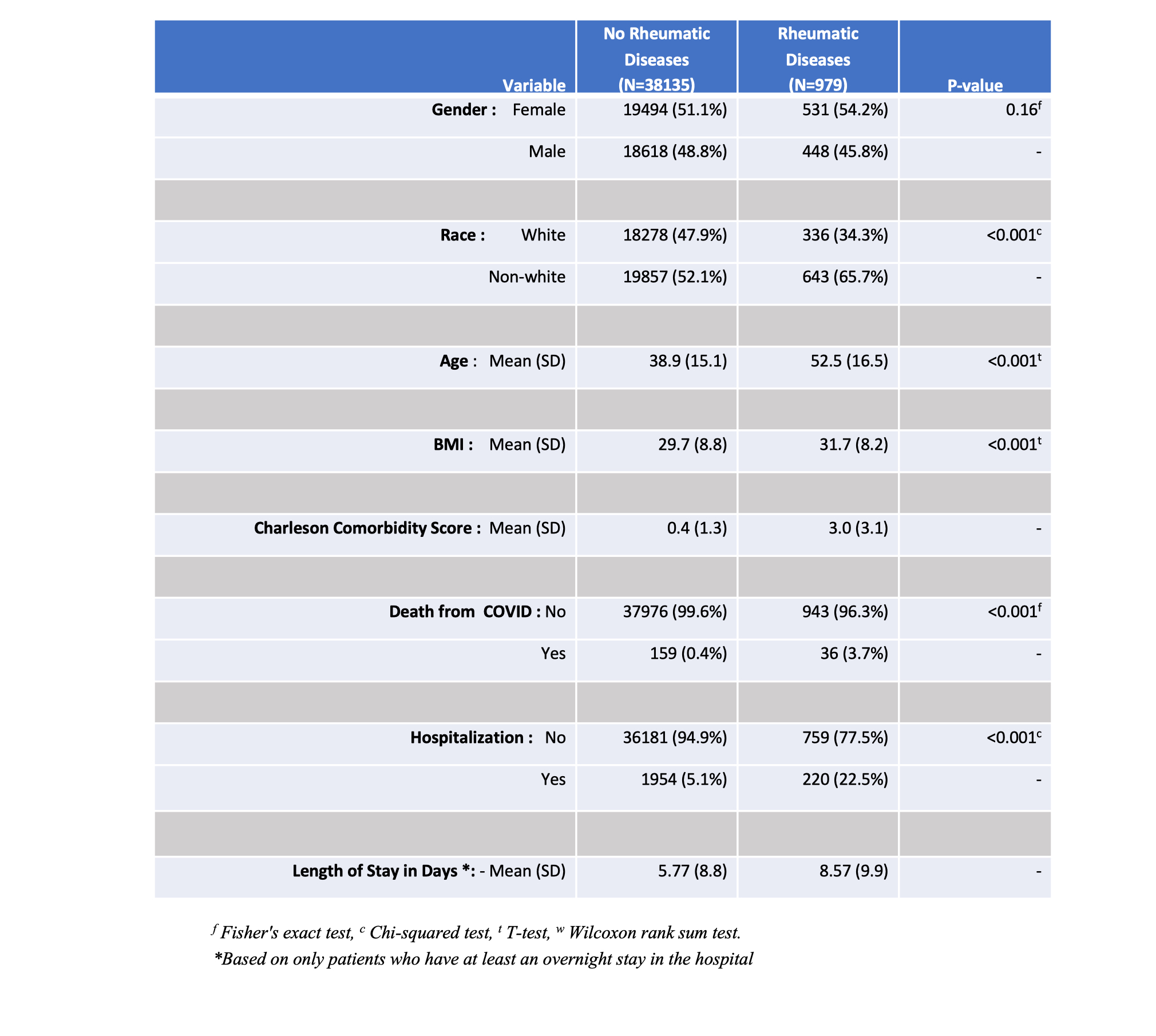
Results: The University of Utah COVID-19 database identified 39,114 patients with confirmed COVID-19 infection with 195 deaths (0.5 %) from January 1, 2020 to March 26, 2021. 979 patients were identified with rheumatic diseases (2.5%) (see Table 1). In weighted and unweighted multivariable logistic regression, rheumatic disease was associated with higher odds of death (OR 1.5, 95% CI 1.01 to 2.22) and (OR 1.57, 95% CI 1.02 to 2.39), respectively. Rheumatic disease was also associated with higher odds of hospitalization (OR 1.77, 95% CI 1.48 to 2.13). Independent factors associated with COVID-19-related death were age (OR 1.08, 95% CI 1.07 to 1.1), male sex (2.52, 1.83 to 3.47) and CCI (1.27, 1.21 to 1.32). In the immunosuppressants subgroup analysis, there was no evidence for a difference in odds of death in glucocorticoids (OR 0.65, 95% CI 0.23 to 1.84), conventional synthetic DMARDs (OR 0.39, 95% CI 0.13 to 1.22) and biological DMARDs (OR 1.13, 95% CI 0.12 to 10.43).
Conclusion: Among patients with COVID-19 infection, persons with rheumatic diseases have an increased odds of death and hospitalization compared to persons without rheumatic diseases.
To cite this abstract in AMA style:
Albalwi M, Brintz B, Beddhu S, Wei G, Thomas J. COVID-19 Mortality and Hospitalization Risk in Patients with Rheumatic Diseases: A Single Center Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/covid-19-mortality-and-hospitalization-risk-in-patients-with-rheumatic-diseases-a-single-center-retrospective-cohort-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/covid-19-mortality-and-hospitalization-risk-in-patients-with-rheumatic-diseases-a-single-center-retrospective-cohort-study/