Background/Purpose:
The frequency of admission to rehabilitation varies among countries but also among diagnosis groups. So far research describing and comparing the rehabilitation in various diagnosis groups using a similar set of endpoint measures is missing.
Aim: To describe the course and outcome of rehabilitation care in different rheumatological diagnosis groups.
Methods:
Multicenter prospective observational study in 4 North-European countries (18 study sites) including patients with various rheumatic diseases admitted for rehabilitation. Assessments were done at admission, discharge and after 6 and 12 months. Assessments included pain, fatigue (numeric rating scales, NRS, 0-10), physical functioning (Health Assessment Questionnaire, HAQ, 0-3), Quality of Life (EQ-5D and SF-36). In addition, at baseline sociodemographic and health characteristics were recorded. Moreover, the setting and duration of the rehabilitation were registered. Comparisons of baseline characteristics among diagnosis groups were made using multivariate or logistic regression analysis. Changes over time were analysed within diagnosis groups using analysis of variance, including all available data.
Results:
1215 patients were evaluated. The different diagnosis groups were Rheumatoid arthritis, 418 patients, Spondylarthropathies, 300 patients, systemic rheumatic diseases, 104 patients, unspecified arthritis, 22 patients, fibromyalgia/chronic pain 45 patients, non-inflammatory back pain, 26 patients and osteoarthritis 119 patients. 181 patients participated in rehabilitation post large joint surgery of which 171 patients were diagnosed with osteoarthritis and the 10 remaining patients had an inflammatory arthritis.
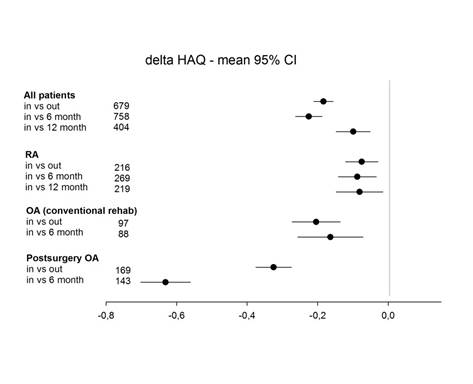
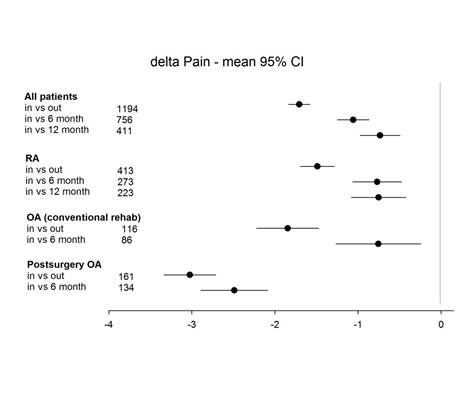
In all diagnosis groups, patients improved significantly between baseline and the discharge assessments in pain, fatigue, HAQ. The mean change in pain was -1.7 (confidence interval (CI) -1.8 – -1.6), in fatigue -1.6 (CI -1.7 – -1.5) and in HAQ -0,18 (CI -0.21 – -0.16). After 6 months the mean change from baseline in pain was -1.1 (CI -1.2 – -0.9), in fatigue -0.7 (CI -0.9 – -0.5) and in HAQ -0.22 (CI -0.26 – -0.19). The improvements were similar in all diagnosis groups except for the post-surgery osteoarthritis patients where the improvements were remarkably higher.
Conclusion:
Using a standardized framework across diagnosis groups we were able to demonstrate improvement after rehabilitation within 10 rheumatological diagnosis groups. The use of similar endpoint measures in national registries is advocated. It is of importance to register all treatments apart from drugs.
Disclosure:
E. Lindqvist,
None;
M. Grotle,
None;
K. Hoerslev-Petersen,
None;
T. P. M. Vliet Vlieland,
None;
A. B. I. Bremander,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/course-and-outcome-of-rehabilitation-care-in-different-rheumatological-diagnosis-groups-a-descriptive-study-using-the-star-etic-registry/