Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is associated with significant health care utilization, medical costs, and increased risk of hospitalization. We aimed to characterize the reasons for admission that are associated with the highest costs of hospitalization in patients with SLE compared to those without SLE.
Methods: We retrospectively reviewed the National Inpatient Sample, which approximates a 20-percent stratified sample of discharges from U.S. community hospitals. We included all adult (age ≥18) hospitalizations between the years 2017-2021. Patients were classified as having SLE if they had either a principal or secondary International Classification of Disease (ICD-10-CM) diagnosis code of M32. Discharge-level weights were utilized to produce national estimates and calculate descriptive statistics. Aggregate and median costs of hospitalization were estimated from total charges using hospital-level cost-to-charge ratios as provided as part of the Healthcare Cost and Utilization Project (HCUP). All costs were adjusted for inflation using the Personal Health Care Index for hospital care as constructed by the Centers for Medicare & Medicaid Services. Costs were stratified by body system associated with the principal diagnosis as defined by the Clinical Classifications Software Refined for ICD-10-CM diagnoses (CCSR), a tool developed through HCUP. All analyses were performed using Stata version 18.0 and an alpha of 0.05 was used.
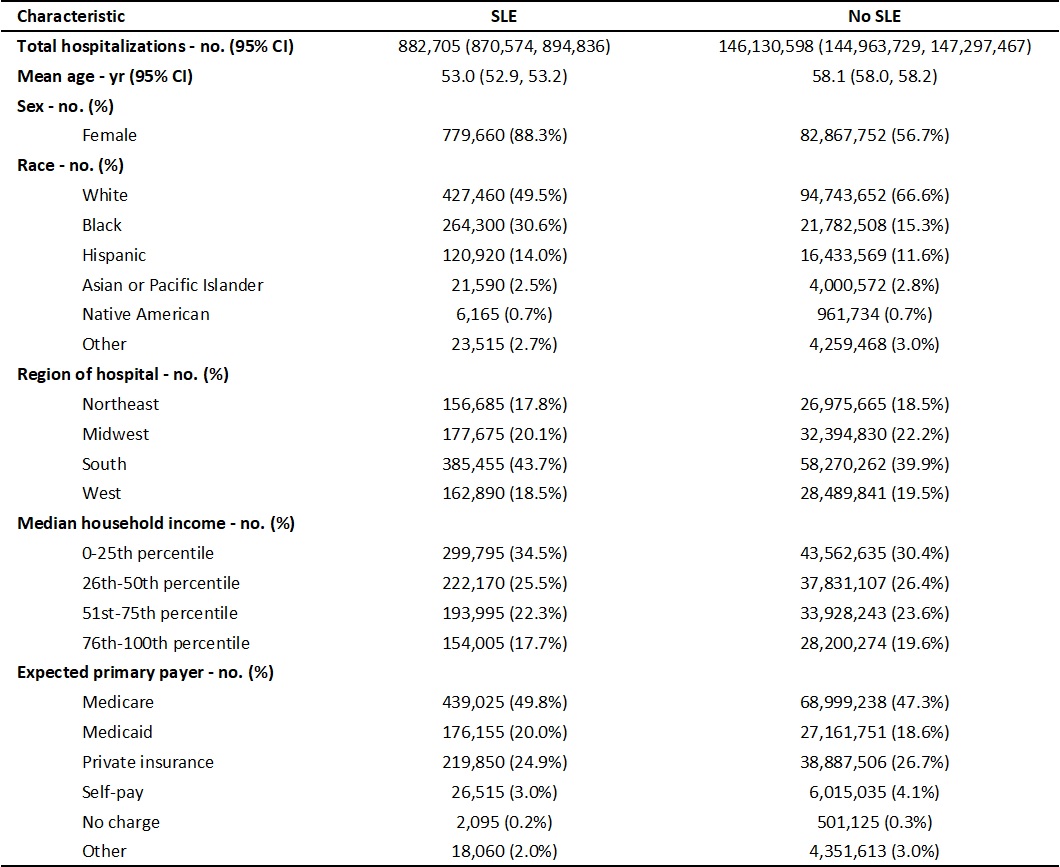
Results: Our cohort included an estimated 882,705 adult patients with SLE and 146,130,598 patients without SLE. Patients with SLE were more likely to be younger, female, of Black race, hospitalized in the South, in the lowest income quartile, or to have a primary payer of Medicare or Medicaid compared to patients without SLE (table 1).
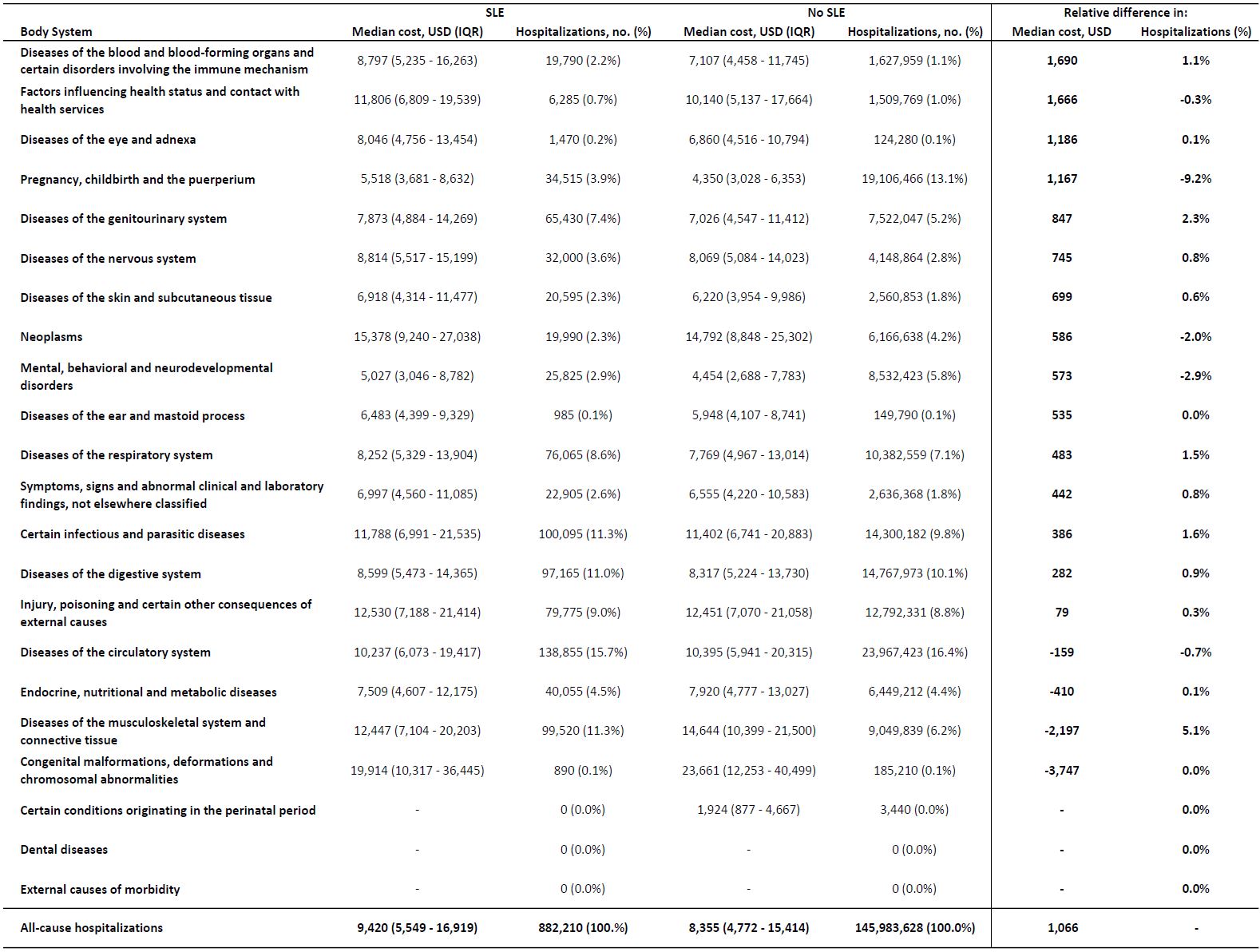
The median cost of hospitalization for patients with SLE was $9,420, versus $8,355 for patients without SLE (table 2). Congenital disorders resulted in the highest median cost for both groups ($19,914 vs $23,661), though were few in frequency and similar in both groups (0.1% vs 0.1%). Of diagnoses with >1% frequency, the conditions with highest relative median cost between patients with and without SLE were hematologic ($8,797 vs $7,107), obstetric ($5,518 vs $4,350), and genitourinary ($7,873 vs $7,026).
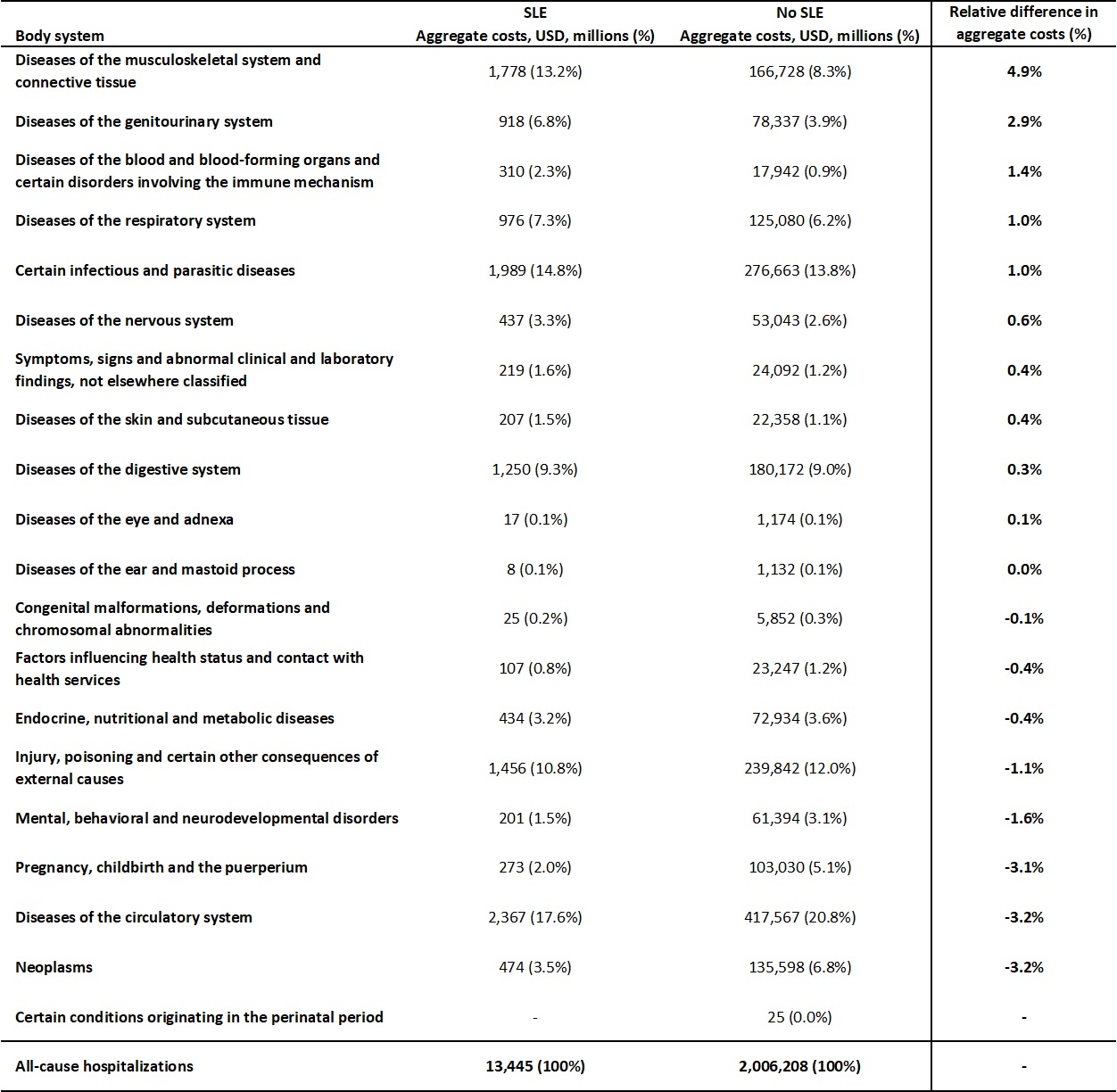
Total costs of all-cause hospitalizations for patients with SLE were $13,445 million (MM), versus $2,006,208 MM for those without SLE (table 3). Between patients with and without SLE, the conditions with the greatest percentage difference of aggregate costs were musculoskeletal (13.2% vs 8.3%), genitourinary (6.8% vs 3.9%), and hematologic (2.3% vs 0.9%). Diseases of the circulatory system accounted for the largest share of costs in both groups (17.6% vs 20.8%).
Conclusion: Hospitalizations of patients with SLE were associated with higher median costs than those of patients without SLE. The distributions of aggregate and median costs across principal diagnoses differ notably between patients with and without SLE, likely a result of the multisystemic complications of this illness. These disparities highlight potential targets for future systems-level interventions to prevent expensive hospitalizations in patients with SLE.
Costs estimates are presented as median with interquartile range (IQR). Costs are represented as US dollars (USD) after adjusting for inflation using the Personal Health Care Index for hospital care. Hospitalizations with an invalid or missing principal diagnosis code were excluded from the analysis.
Cost estimates are presented in aggregate and as a percentage of total all-cause hospitalizations. Costs are represented as millions of US dollars (USD) after adjusting for inflation using the Personal Health Care Index for hospital care. Hospitalizations with an invalid or missing principal diagnosis code were excluded from the analysis.
To cite this abstract in AMA style:
Blau B, Gripp K, MacLean C, Mehta B. Costs of Hospitalization in Patients with SLE: An Analysis of the National Inpatient Sample [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/costs-of-hospitalization-in-patients-with-sle-an-analysis-of-the-national-inpatient-sample/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/costs-of-hospitalization-in-patients-with-sle-an-analysis-of-the-national-inpatient-sample/