Session Information
Date: Sunday, October 26, 2025
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Up-to-date information on the cost-of-illness of psoriatic arthritis (PsA) is important for healthcare/social insurance system budgeting and to highlight unmet needs in PsA care. Here, we aimed to estimate societal costs (for healthcare/work disability) during one year (yr) from diagnosis among all working-age (18-64yr) individuals diagnosed with PsA in Sweden 2016-2019, and to relate these to costs during the preceding yr and in the general population (GP).
Methods: Newly diagnosed PsA patients were identified from the Swedish National Patient Register (NPR) and the Swedish Rheumatology Quality register (SRQ): ≥1 ICD-10 code for PsA (L40.5/M07.0-M07.3) as main diagnosis from rheumatology/internal medicine units in NPR or PsA diagnosis registered in SRQ 2016-2019, and no prior such diagnoses. Each PsA case was matched by sex/age/county to 5 GP comparators without PsA according to NPR/SRQ, and costs (inflation-adjusted to 2019 US Dollars [$]) from 1yr before to 1yr after PsA diagnosis (and the same period for comparators) were estimated. Costs for all dispensed prescription drugs were retrieved from the Prescribed Drug Register, while intravenous bDMARDs were priced based on doses in SRQ. For specialized (non-primary) out-/inpatient care (retrieved from NPR), costs were calculated via the Swedish 2019 Diagnosis Related Group (DRG) system. Work disability costs were estimated as accumulated net sick leave/disability pension days (Social Insurance Agency) multiplied with the average daily salary (plus social fees) in Sweden 2019. Despite skewness, costs are reported as arithmetic means, considered most informative for cost studies. Cost comparisons between PsA and comparators were done by non-parametric bootstrapping, accounting for the matched design; between subsets of PsA by Mann-Whitney U-test; and between years by Wilcoxon’s matched-pair signed-rank test.
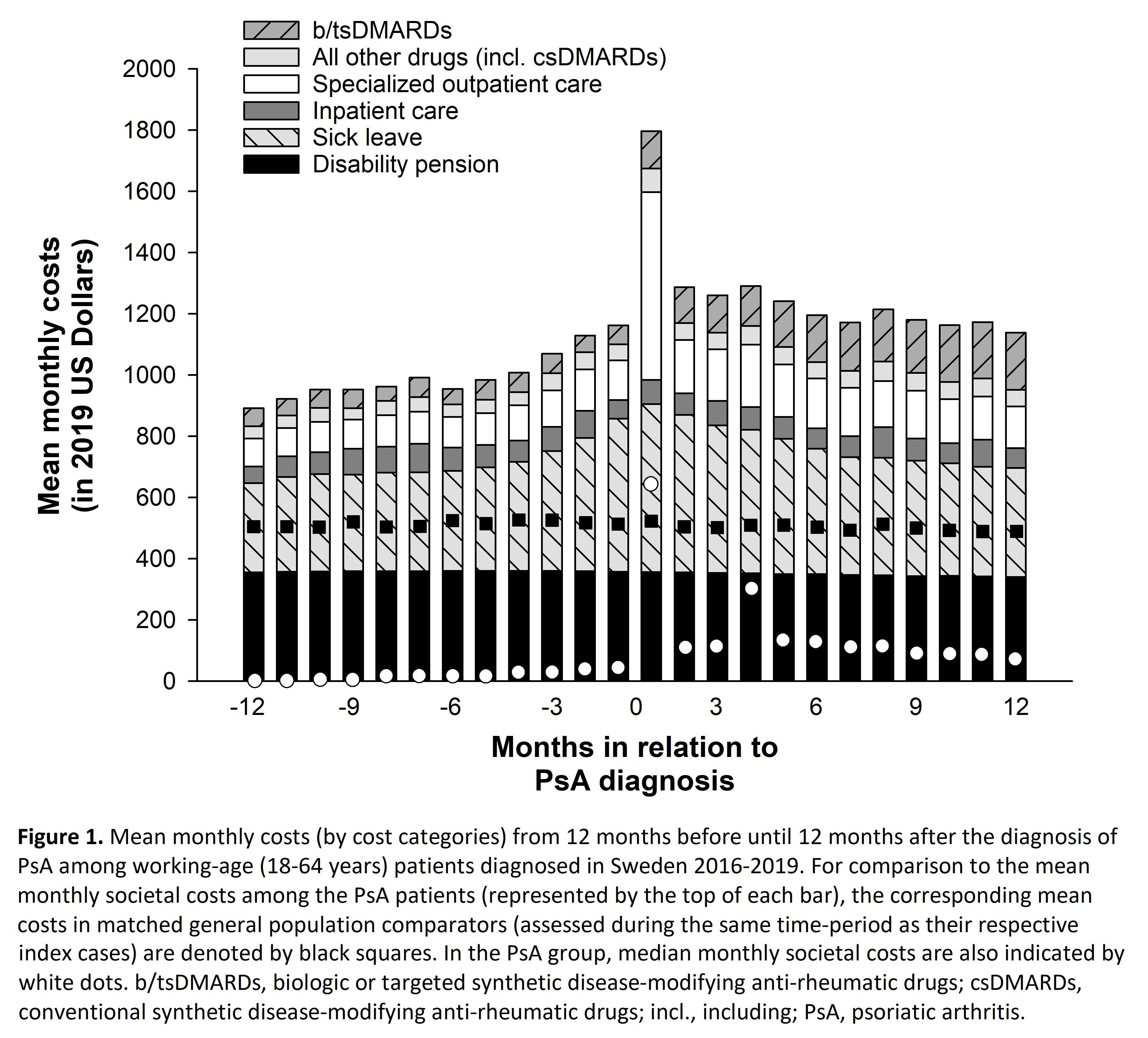
Results: During the yr following diagnosis, societal costs were significantly higher in PsA (n=5196; mean cost $15 101) than in the GP comparators (n=25 740; mean cost $6051; mean between-group difference: $9048), with elevations of all cost categories and dominated by work disability costs (61% of societal costs in PsA; Table). Costs were highly skewed, with 11% of cases accounting for 50% of all societal costs in PsA. The monthly costs for all categories (except inpatient care) were significantly elevated compared to the GP already 12 months prior to PsA diagnosis. Costs increased gradually (mainly due to rising sick leave) to a peak at diagnosis, and then slightly decreased during the following 11 months (Figure 1). Except for inpatient care and disability pension costs, all annual cost categories increased significantly from the yr before to the yr after diagnosis (Figure 2). Societal costs were higher in females and individuals with lower education (Figure 2).
Conclusion: Already in the year following diagnosis, PsA (at a group level) imposes a substantial health economic burden on society, with societal costs 2.5 times higher than in the GP and with work disability as the dominant cost driver. Whether earlier diagnosis/interventions could bring about a more favorable cost trajectory should be a focus of future studies.
To cite this abstract in AMA style:
Wittgren S, Exarchou S, Di Giuseppe D, Lindström U, Olofsson T, Jacobsson L, Askling J, Karlsson Wallman J. Cost-of-Illness Among Newly Diagnosed Patients with Psoriatic Arthritis in Sweden [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/cost-of-illness-among-newly-diagnosed-patients-with-psoriatic-arthritis-in-sweden/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cost-of-illness-among-newly-diagnosed-patients-with-psoriatic-arthritis-in-sweden/

.jpg)
.jpg)