Session Information
Date: Sunday, November 8, 2015
Title: Osteoarthritis - Clinical Aspects: Treatments and Epidemiology
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: The US spends over $1 billion
annually on opioids for persons with knee OA. We evaluated whether the use of opioids
offers good value for money by conducting a formal cost-effectiveness analysis
of the use of tramadol or oxycodone in OA patients.
Methods: We used the Osteoarthritis Policy
Model, a validated computer simulation of knee OA, to evaluate long-term
clinical and economic outcomes of knee OA patients with mean age 60 and no
prevalent comorbidities, whose pain persists after initial treatment with non-steroidal
antiinflammatory drugs (NSAIDs), physical therapy (PT), and corticosteroid
injections. We evaluated 3 strategies: 1) opioid-sparing (OS, acetaminophen as
needed until total knee arthroplasty [TKA]); 2) tramadol (T); and 3) tramadol
followed by oxycodone for those who failed tramadol (T+O). Toxicity and efficacy
were estimated from published literature. Mean WOMAC Pain change was 15 points
for tramadol and 16 for oxycodone. Annual costs for tramadol ($600) and
oxycodone ($2,700) included drug costs (Red Book), office visits, and, for
oxycodone, diversion. Toxicities included gastrointestinal (GI) and cardiovascular
(CV) events. Based on published literature, in the base case analysis we decreased
the efficacy of TKA in strategies T and T+O by 10%. We adopted a societal
perspective, discounting outcomes at 3%/year, and assumed a willingness to pay
(WTP) threshold of $100,000 per quality adjusted life year (QALY). Strategies
with incremental cost-effectiveness ratios (ICERs) below WTP were considered cost-effective.
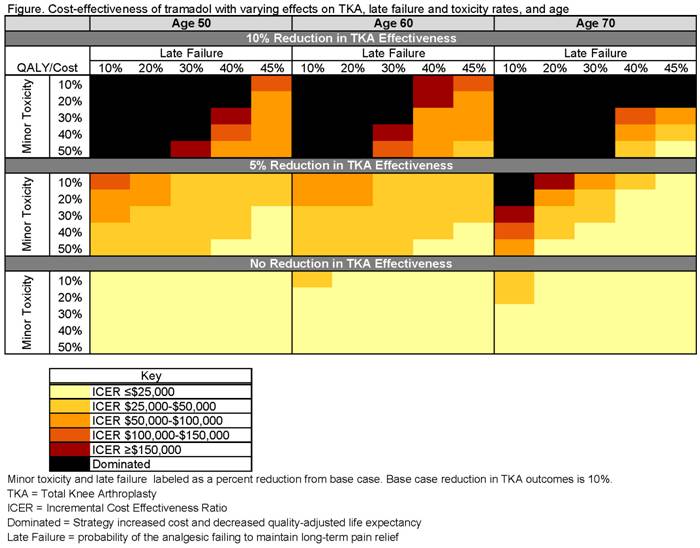
We conducted sensitivity analyses on the impact of opioid use on TKA outcomes, age
at opioid initiation, and toxicity and discontinuation rates.
Results: In the base case, tramadol-treated patients were on tramadol for
2.4 years and oxycodone-treated patients were on oxycodone for 2.9 years, on
average. The T and T+O strategies led to reduction in TKA use by 4% and 10%
respectively and revision TKA use by 24% and 40%. In the base case, both opioid-based
strategies increased cost and decreased QALYs compared to the opioid-sparing
strategy. Tramadol cost-effectiveness was highly sensitive to its effects on
TKA outcomes. When efficacy of TKA was reduced by 5% (base case 10%), tramadol
had an ICER of $67,000/QALY (Figure). When TKA was not a treatment option,
tramadol, but not tramadol + oxycodone, became a cost-effective strategy.
Conclusion: Opioids do not appear to be cost-effective
in OA patients if they have an adverse effect on TKA outcomes. Despite
reductions in TKA use, costs of opioids and toxicities led to an overall
increase in cost for the T and T+O strategies compared to OS. Tramadol may be cost-effective
in patients averse to TKA or if additional data show that its effects on TKA
outcomes are minimal. The influence of chronic opioid use on TKA should be
considered a research priority in order to understand the value of opioids in
knee OA treatment.
To cite this abstract in AMA style:
Smith SR, Katz JN, Collins JE, Losina E. Cost-Effectiveness of Opioids for the Treatment of Knee Osteoarthritis: Impact of Chronic Opioid Use on Total Knee Arthroplasty Outcomes [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/cost-effectiveness-of-opioids-for-the-treatment-of-knee-osteoarthritis-impact-of-chronic-opioid-use-on-total-knee-arthroplasty-outcomes/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cost-effectiveness-of-opioids-for-the-treatment-of-knee-osteoarthritis-impact-of-chronic-opioid-use-on-total-knee-arthroplasty-outcomes/