Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is a chronic multi-system autoimmune disease with frequent neuropsychiatric symptoms associated with poor outcomes. Small fiber neuropathy can cause intolerable pain and is an underdiagnosed neurological manifestation of SLE due to a normal or near-normal neurological examination and electrophysiological testing. Indeed, it is not included in the Neuropsychiatric SLE criteria, The purpose of this study was to evaluate the utility of corneal confocal microscopy (CCM) in identifying small nerve fiber damage in patients with SLE.
Methods: A cross-sectional study conducted over one year, included 59 SLE patients and 17 healthy controls. Inclusion criteria were adult patients (≥18years old) who satisfy at least four of (ACR) SLE classification criteria. Exclusion criteria were other causes of peripheral neuropathy, corneal trauma, dystrophy, surgery, severe dry eyes or allergy to local anesthetics. Subjects underwent clinical examinations, DN4 questionnaire, CCM, sudomotor function assessment and vibration perception threshold (VPT). The CCM outcome measures were corneal nerve fiber, length and branch density. Basic descriptive statistics were reported as mean ± SD. The Pearson χ2 test was used to compare categorical variables. For all evaluations, a two-sided P value of less than 0.05 was considered statistically significant.
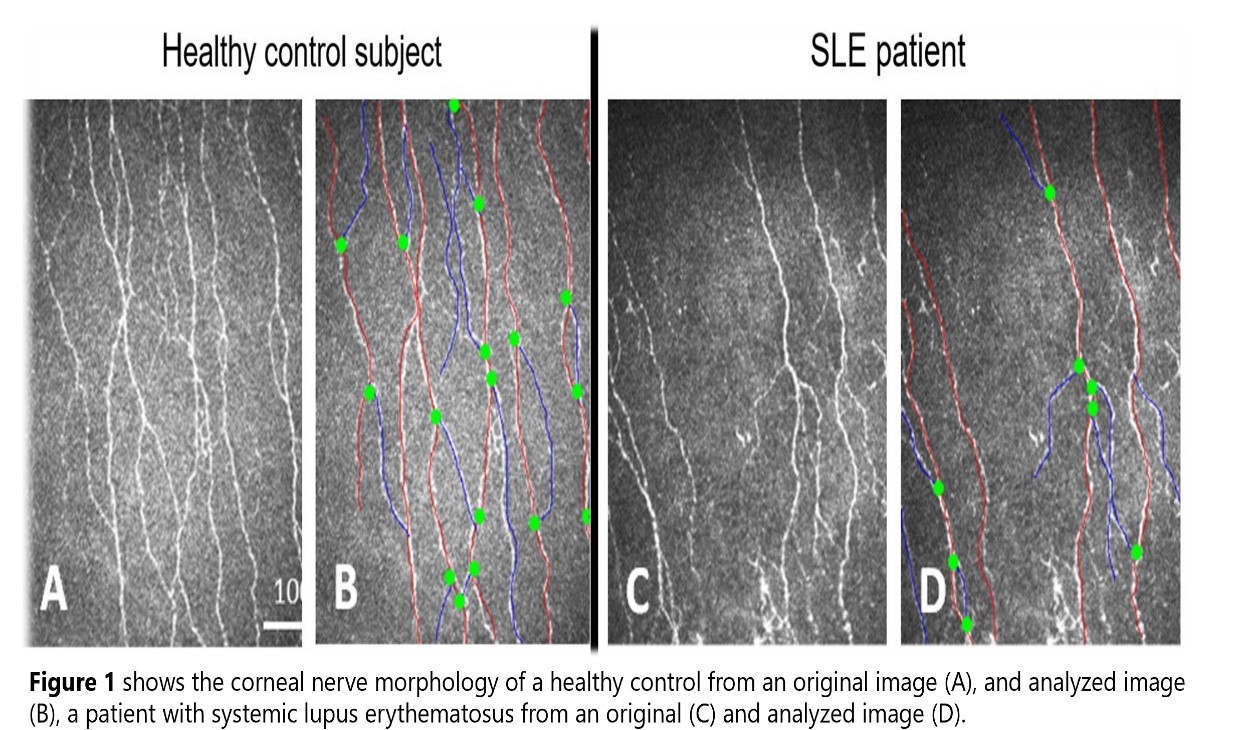
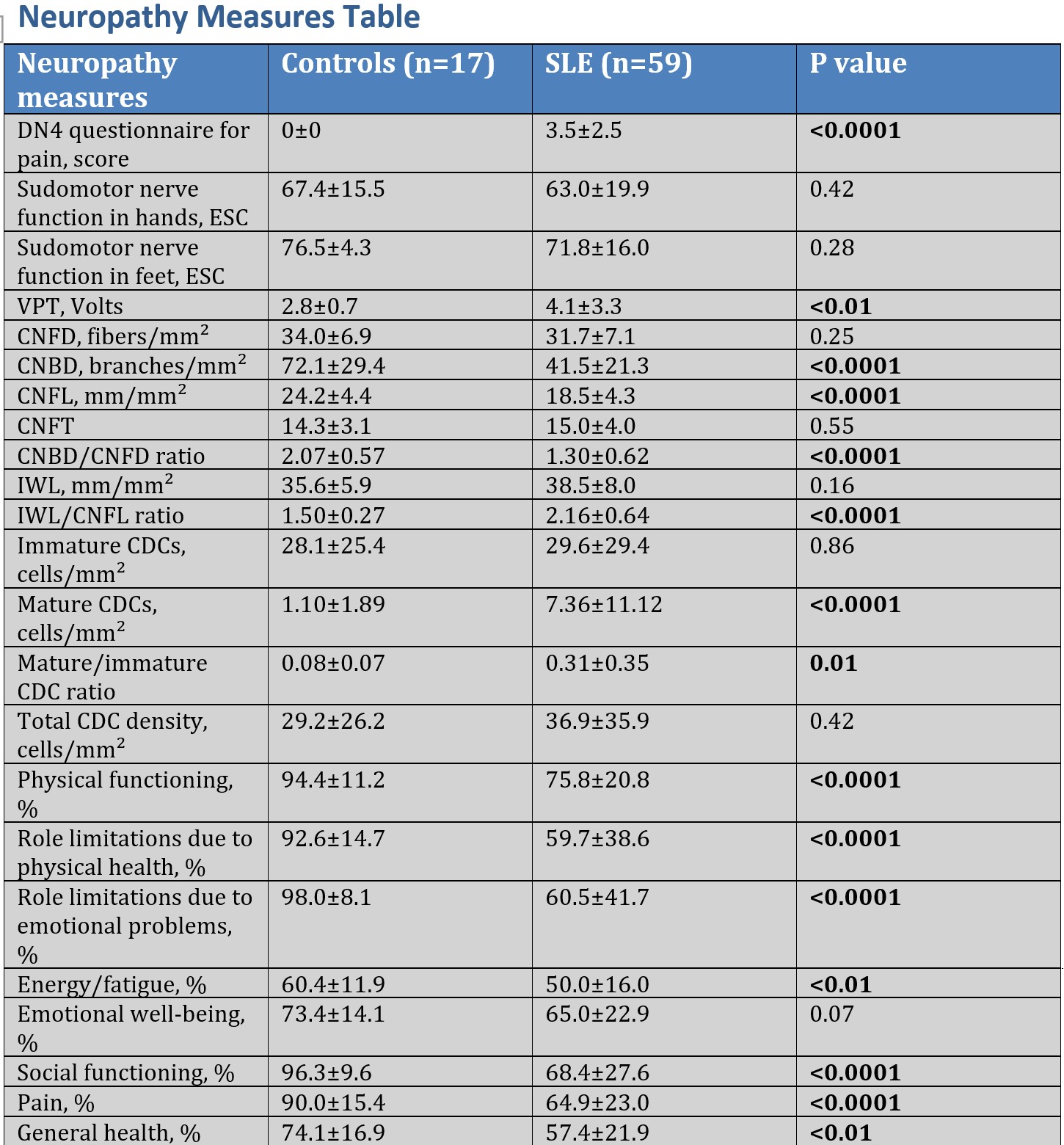
Results: There were no differences between SLE patients and controls for age (P = 0.07) and sex (P = 0.09). The mean time from the initial diagnosis of SLE was 8.7 ± 6.6 years. 37of 59 (62.7%) patients had moderate to high disease activity. Participants with SLE (n=59) had Lower corneal nerve branch density (CNBD) (P< 0.0001), lower fiber length (CNFL) and CNBD/CNFD ratio (P< 0.0001),Higher mature dendritic cell (DC) density (P< 0.0001), Higher VPT, Higher DN4 questionnaire for pain score, Comparable corneal nerve fiber density (CNFD) (P=0.25) and immature DC density (P=0.86) (Fig. 1,Table 1) ,Those with active SLE (n=37, 62.7%) had significantly lower Corneal branch-to-fiber ratio (P< 0.05) .Comparable CNFD (P=0.47), CNBD (P=0.31), CNFL (P=0.75), mature DC density (P=0.66), and immature DC density (P=0.78) compared to those with inactive SLE (n=22, 37.3%).Those with SLE and continuous pain (n=10, 17.2%) had significantly lower CNFD (P< 0.01) and CNFL (P< 0.05) ,Comparable mature and immature DC density (P=0.37-0.99) compared to those with transient (n=12, 20.7%) or recurrent pain (n=36, 62.1%). SLE patients reported more limitations in their daily roles due to physical health concerns, emotional issues, higher levels of fatigue, less social interaction, more pain, and a lower general health compared to healthy controls (P< 0.01-0.0001), with similar emotional well-being (P=0.07). In regression analysis, physical activity difficulties were significantly associated with reduced CNBD, CNFL, and CNBD/CNFD ratio (P< 0.05).
Conclusion: Corneal confocal microscopy (CCM), A non-invasive imaging modality detects small nerve fiber damage in patients with SLE, particularly in those with neuropathic pain encouraging the utility of CCM as a surrogate marker of neurodegeneration for SLE.
To cite this abstract in AMA style:
Gharib M, Baloglu G, Osman S, A.Malik R, Alemadi S. Corneal Confocal Microscopy: An Ophthalmic Imaging Biomarker for Small Fiber Neuropathy in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/corneal-confocal-microscopy-an-ophthalmic-imaging-biomarker-for-small-fiber-neuropathy-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/corneal-confocal-microscopy-an-ophthalmic-imaging-biomarker-for-small-fiber-neuropathy-in-systemic-lupus-erythematosus/