Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: While it is well accepted that congenital heart block (CHB) and neonatal annular rash are highly associated with maternal anti-Ro60 and 52 autoantibodies, the contribution of these auto-reactivities to other adverse pregnancy outcomes (APOs) is often discussed during pregnancy counseling with limited data available. Moreover, it is unknown whether titers or specificities of these putative antibodies alone or in the setting of additional maternal factors such as ethnicity, race, and/or health status influence APOs. Accordingly, this study was initiated to address these considerations leveraging a large multi-center prospective cohort of pregnancies (aimed at identifying emergent CHB) in which women were recruited solely on the basis of a known positive test for anti-Ro antibodies.
Methods: 216 pregnant patients recruited across the U.S. with anti-Ro antibodies present based on commercial testing at local laboratories were enrolled prior to 18 weeks gestation and prospectively followed. Anti-Ro antibody titers were confirmed at a central research laboratory by ELISA using native Ro60 and recombinant Ro52. All mothers provided self-reported demographic data, and maternal health status was assessed by clinical interviews and patient medical records. APOs reported to the DSMB included premature delivery < 37 weeks, small for gestational age defined as birth weight < 5th percentile, neonatal or fetal death > 12 weeks, pre-eclampsia at any time, and/or severe oligohydramnios. CHB was considered a separate outcome from APO.
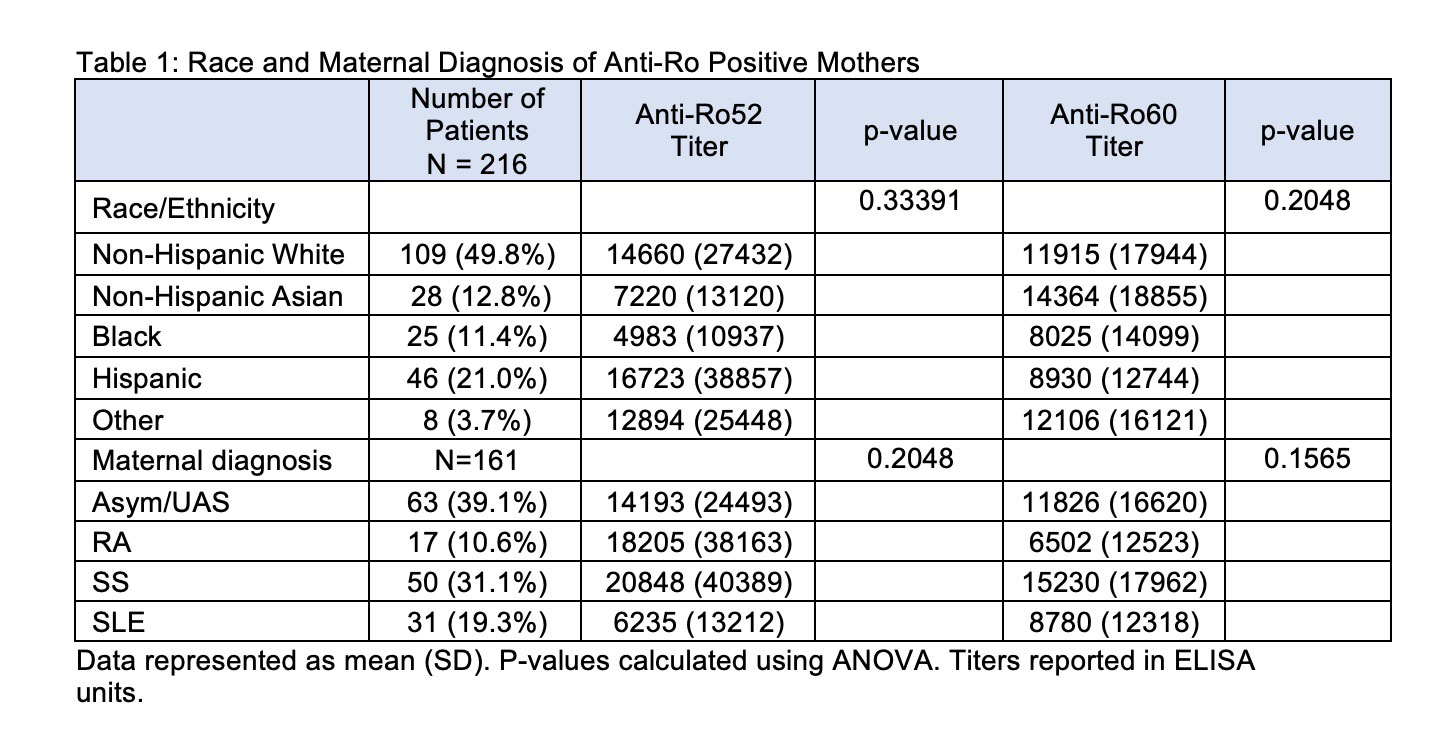
Results: Anti-Ro60 and anti-Ro52 titers were independent of race and ethnicity (Table 1). In addition, average titers did not differ by maternal diagnosis which was determined for 161 patients and included: asymptomatic/Undifferentiated Autoimmune Syndrome (UAS) (N = 63), Sjögren’s Syndrome (SS) (N = 50), Systemic Lupus Erythematosus (SLE) (N = 31), and Rheumatoid Arthritis (RA) (N = 17) (Table 1). Of the enrolled patients, 109 completed pregnancies with APOs occurring in 20 (23%) and CHB occurring in 4 patients. Mean titers of anti-Ro60 and anti-Ro52 did not associate with APOs (mean +/- SD, anti-Ro60: no APOs 9404 +/- 13514; with APOs 10930 +/- 14412; p-value = 0.6537. anti-Ro52: no APOs 13690 +/- 31068; with APOs 21356 +/- 42203, p-value = 0.3610). In contrast to antibody titers and specificities, the maternal diagnosis did influence APOs. Mothers with established SLE were significantly more likely to have APOs than any of the other disease groups (P< 0.006) (Table 2).
Conclusion: The titer and specificity of anti-Ro antibodies did not segregate based on ethnicity, race, or maternal diagnosis. Moreover, APOs were not influenced by antibody titers or specificities, but rather by the maternal diagnosis of SLE.
To cite this abstract in AMA style:
Fraser N, Masson M, Deonaraine K, Carlucci P, Phoon C, Roman A, Izmirly P, Saxena A, Belmont M, Penfield C, Lee Y, Nusbaum J, Solitar B, Malik F, Rackoff P, Haberman R, Acherman R, Sinkovskaya E, Albuhamad A, Makhoul M, Satou G, Pinto N, Moon-Grady A, Howley L, Levasseur S, Matta J, Lindblade C, Rubenstein A, Haxel C, Kohari K, Copel J, Strainic J, Doan T, Bermudez-Wagner K, Sheth S, Killen S, Tacy T, Kaplinski M, Drewes B, Clancy R, Cuneo B, Buyon J. Contribution of Antibody Titers/Specificities to Adverse Pregnancy Outcomes in a Multicenter Prospective Study of anti-Ro Positive Mothers [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/contribution-of-antibody-titers-specificities-to-adverse-pregnancy-outcomes-in-a-multicenter-prospective-study-of-anti-ro-positive-mothers/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/contribution-of-antibody-titers-specificities-to-adverse-pregnancy-outcomes-in-a-multicenter-prospective-study-of-anti-ro-positive-mothers/