Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Most prior studies of contraception in women with rheumatic disease focused on academic centers. In this study of non-academic rheumatology practices, we sought to identify the frequency of contraceptive use, types of contraceptives, and variations between sites and based on the woman’s race/ethnicity, age, and rheumatic diagnosis.
Methods: In 2023, three community rheumatology practices, each with a single clinic with multiple providers located in the South, Southeast, and Mid-Atlantic regions documented contraception in women of reproductive age. The study population included all visits for women ages 18-44. Persons of color (POC) include all non-White, non-Hispanic women based on the race and ethnicity data reported by the clinics. SLE diagnosis was defined by the ICD-10 code billed at the visit and contraception was categorized by the most effective method reported for each woman. To account for multiple comparisons, we set statistical significance at p< 0.01.
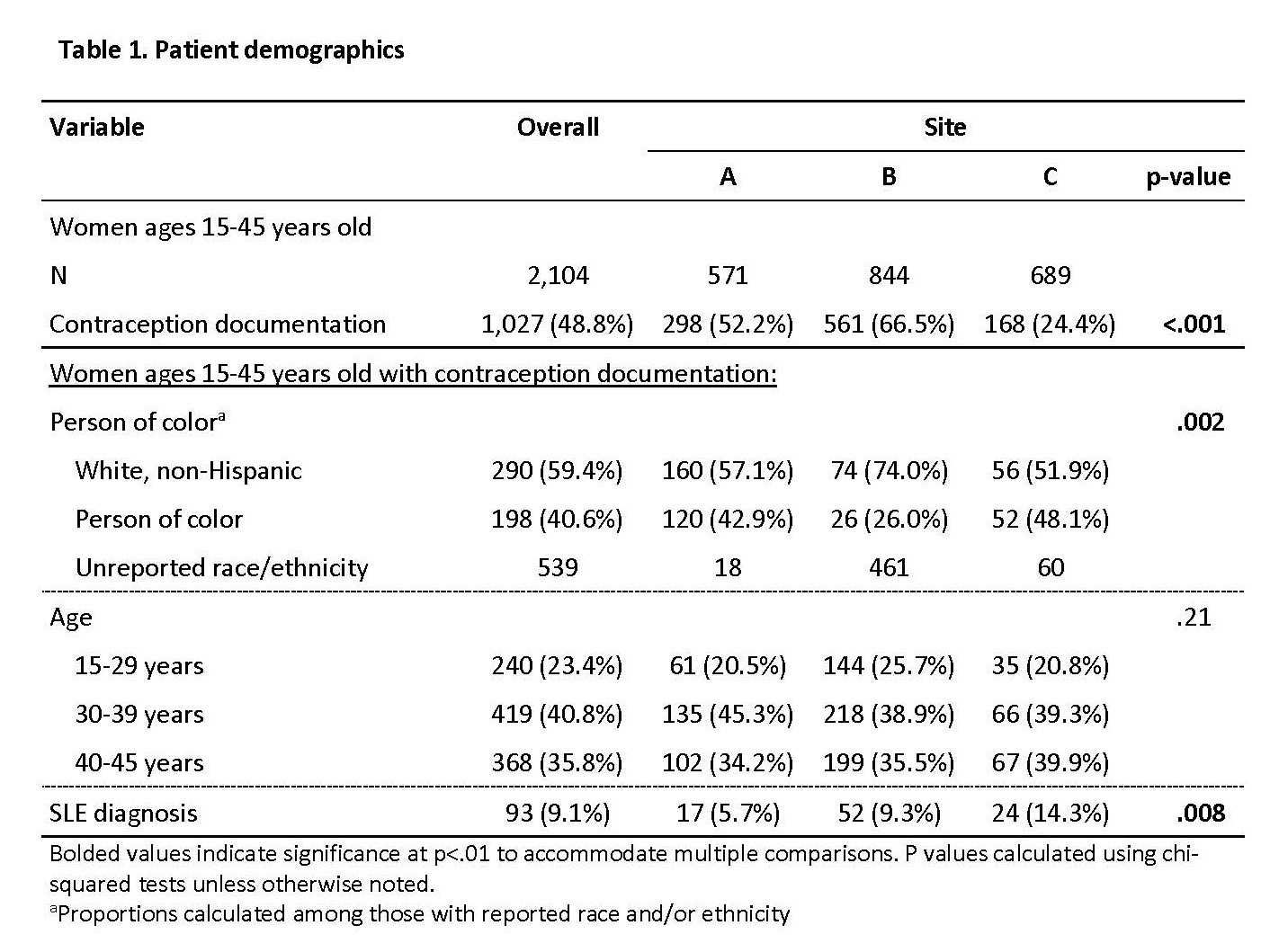
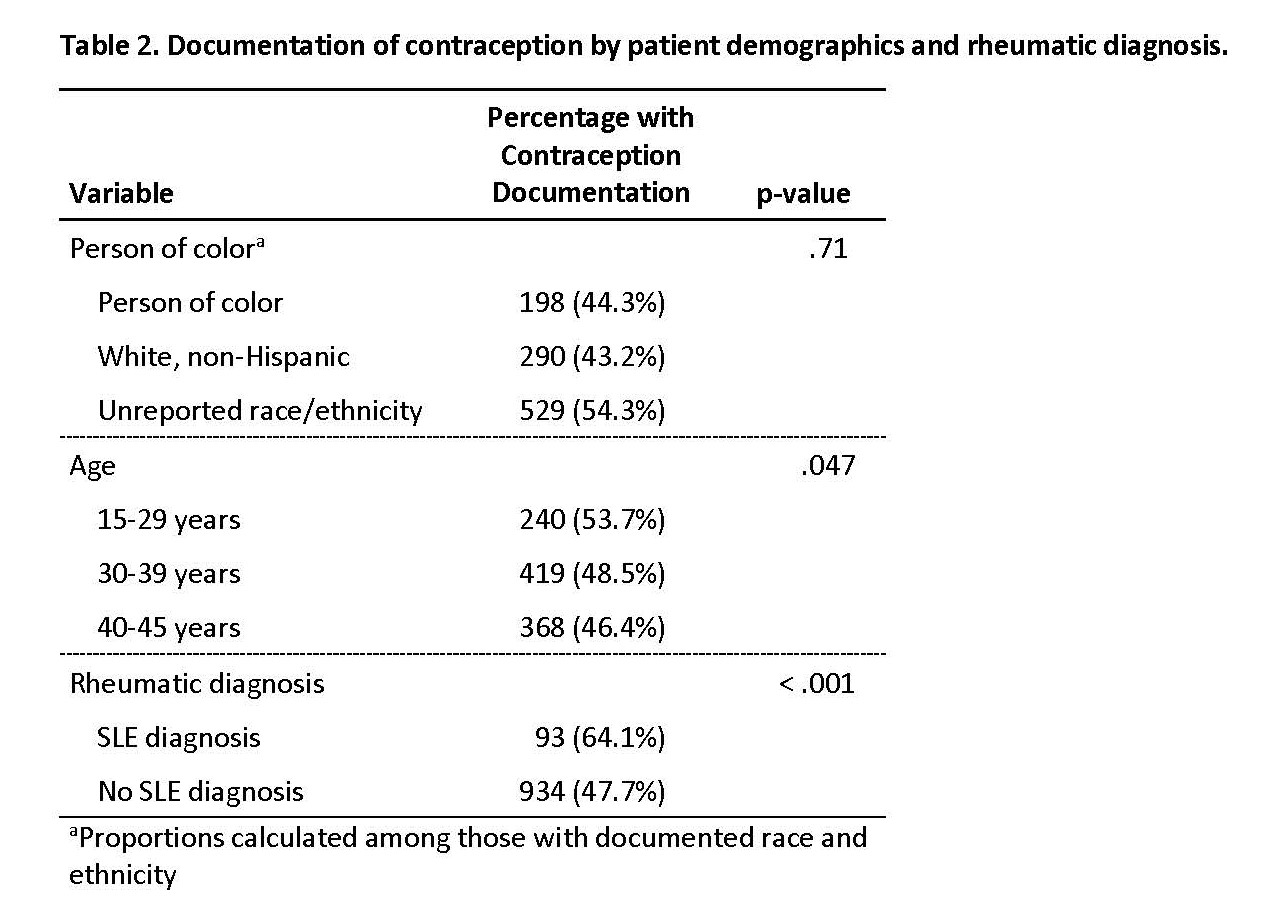
Results: 2,104 women had a clinic visit during this period and 1,027 (48.8%) had contraception documented. Race and ethnicity were missing for many patients, but 40.6% with recorded race and/or ethnicity were POC, the majority of whom were Black. Of those with contraception documentation, the frequency of POC and SLE, but not age, varied by clinic (Table 1). Overall, contraception documentation did not depend on the woman’s age or race/ethnicity, but women with SLE were more likely to have contraception documented (Table 2).
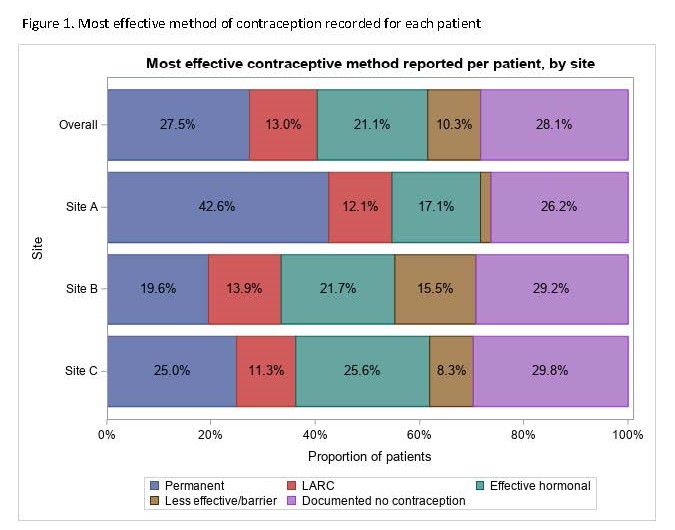
Between 26.2-29.8% of women in every clinic reported not using contraception (Figure 2). Effective hormonal contraceptives were used by 17.1-25.6% of women; LARC by 11.3-13.9% of women. More variability between clinics was found for less effective/barrier methods (2.0-15.5%) and permanent contraception (19.6-42.6%). Hysterectomy was four times as common in one clinic (18.1%) compared to the other two (4.1-4.2%, p-value< 0.001).
The frequency of any contraception use did not vary by age. Compared to women 30-39 and 40-45, women under 30 were significantly more likely to be using hormonal contraception (34.2% versus 10.9-22.4%) and less likely to have permanent contraception (3.3% vs 24.1-46.2%). Contraceptive use did not vary significantly between POC and White women nor women with or without SLE.
Conclusion: The frequency of contraceptive use and types found in this study are similar to those reported in the general population with nearly a third not using contraception. The frequency of contraceptive use, LARC, and hormonal contraceptives was similar between the clinics. We suspect local gynecologic practice may be the cause for the wide difference in the frequency of permanent contraception through hysterectomy. As anticipated, age impacted the type of contraception use, but not race/ethnicity or SLE diagnosis. This study demonstrates the feasibility of systematically asking and documenting contraceptive use in community rheumatology practices. This approach identified a third of the women potentially at risk for an unexpected pregnancy.
To cite this abstract in AMA style:
Clowse M, Chiesa J, Freeman P, Gujar B, Jones K, Jones R, Marslett A, Snyderman A, Zulig L. Contraception in Community Rheumatology Practices [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/contraception-in-community-rheumatology-practices/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/contraception-in-community-rheumatology-practices/