Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatic diseases are prevalent among women of childbearing age; their treatment often requires medications that potentially affect a woman’s fertility and are teratogenic. Prior studies have shown minimal contraception counseling in women receiving high-risk medications and decreased contraception utilization. Our study explores rates of contraception counseling and documentation of contraception use, as well as their type of contraception.
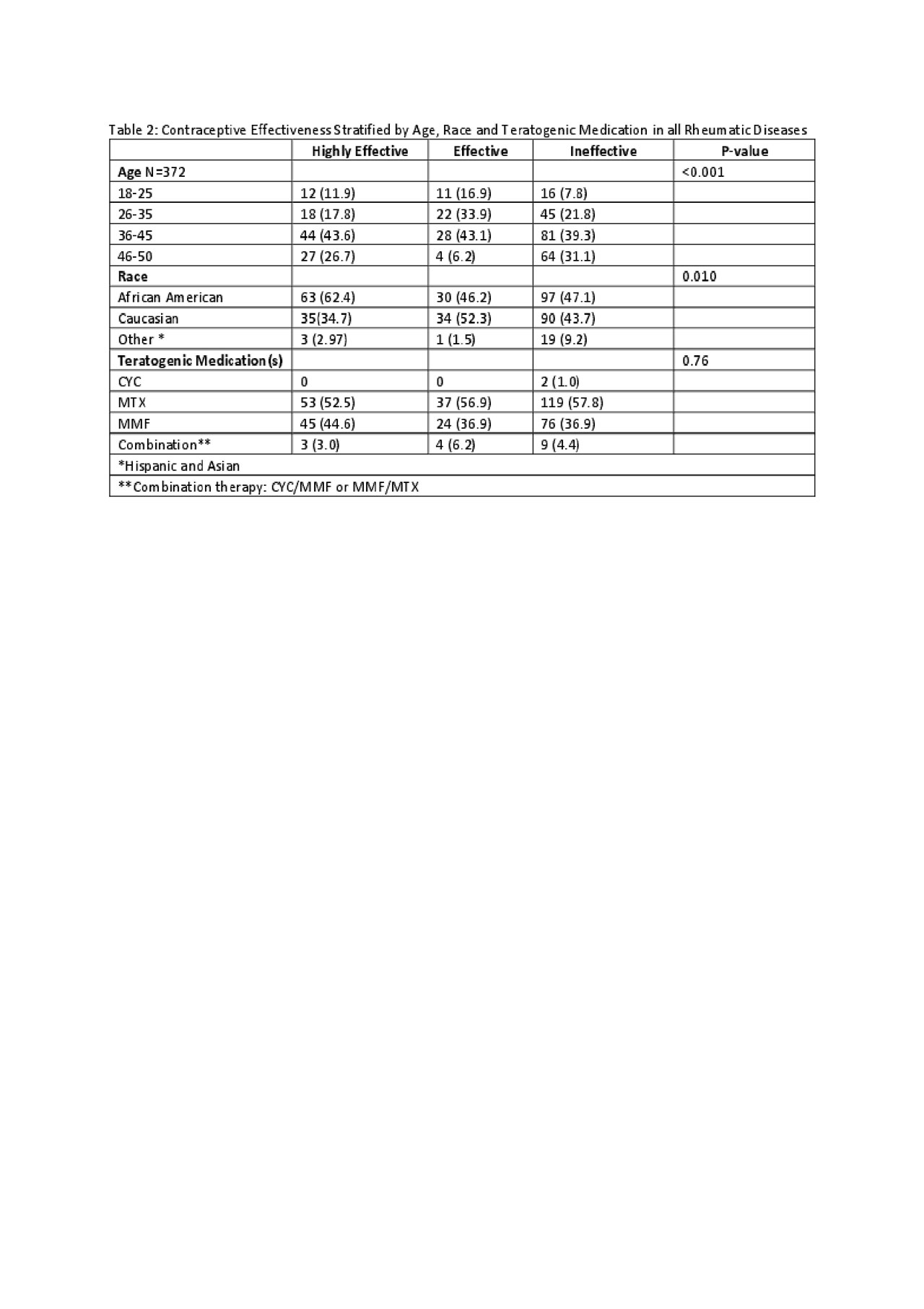
Methods: A retrospective chart review was performed in a university-based Rheumatology clinic. Women ages of 18–50 years who were prescribed mycophenolate mofetil (MMF), methotrexate (MTX), and/or cyclophosphamide (CYC) over a 6-year period with any rheumatic disease were included. 372 of 485 charts reviewed met inclusion criteria. Subject demographics, documentation of contraception type, and counseling were recorded (Table 1). Contraception method was categorized as highly effective (permanent [hysterectomy, tubal ligation] or reversible [IUD, implants, female partners]), effective (OCPs, patch, ring, injection) and ineffective (none, abstinence, condoms). Categorical variables were compared using Fisher’s exact test and ordered logit models were calculated.
Results: The most common teratogenic medication prescribed was MTX (56%), followed by MMF (39%), CYC (0.5%); 4% were taking a combination of these. Median age was 41 years, and majority were African American (51%). Lupus and other related connective tissue diseases (50%) were most represented. Across all rheumatic diseases, documentation of any contraception was 39% and the rate of counseling was 36%. There was a statistically significant relationship between age and race with respect to effectiveness of contraception (p< 0.001 and p=0.010, respectively) (Table 2). Multiple ordered logistic models demonstrated that for patients with contraception counseling, the odds of being on highly effective or effective contraception versus ineffective contraception compared to those without counseling documentation were increased (OR: 1.28, 95% CI: 0.86-1.93). For patients with a documented contraception method, they were more likely to be on highly effective or effective contraception versus ineffective (OR: 5.83, CI: 3.72-9.13). Any reference to contraception (either type or counseling) were more likely to use highly effective or effective contraception (OR: 3.84, CI 2.44-6.04) (Table 3).
Conclusion: Our results demonstrate that a rheumatologist’s recognition of a patient’s need for contraception and clinical documentation of such while on teratogenic medications is the most important predictor of effective contraception method use; the magnitude of its impact is maintained after adjusting for age and race. This study reinforces the importance of increasing both provider and patient education surrounding awareness of contraception needs. Future QI measures to implement interventions that focus on these topics are needed to help improve contraceptive use in young females and increase use of more effective contraceptives in women of all ages on teratogenic medications.
To cite this abstract in AMA style:
Haritha J, Edens C, Ventura I. Contraception Documentation Rates in Women with Rheumatic Diseases on Teratogenic Medications in an Academic Rheumatology Clinic [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/contraception-documentation-rates-in-women-with-rheumatic-diseases-on-teratogenic-medications-in-an-academic-rheumatology-clinic/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/contraception-documentation-rates-in-women-with-rheumatic-diseases-on-teratogenic-medications-in-an-academic-rheumatology-clinic/