Session Information
Date: Tuesday, November 14, 2023
Title: (2387–2424) Vasculitis – Non-ANCA-Associated & Related Disorders Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Relapse is common in giant cell arteritis (GCA) with 40-75% of patients having at least one flare during course of disease. A clinically relevant question for both patients and providers is whether the initial symptoms at GCA diagnosis will be present at time of relapse or whether other clinical features may manifest. Given most cohorts describe both baseline and relapse symptoms in aggregate, evaluation of patient level concordance between initial symptoms and relapse has not been delineated. The purpose of this study was to evaluate the concordance between initial GCA symptoms at diagnosis and first relapse in patients with GCA.
Methods: Two previously described cohorts of patients with GCA were utilized. Cohort 1: 286 patients with biopsy-proven GCA treated with prednisone (no tocilizumab) and Cohort 2: 114 patients with biopsy-proven or imaging-proven GCA treated with tocilizumab. Clinical symptoms at diagnosis and first relapse were grouped into the following categories: constitutional, musculoskeletal (MSK), cranial (non-visual), visual, and large-vessel (LV). Patients could have more than one category present at each time event. Odds ratios and conditional probabilities were calculated.
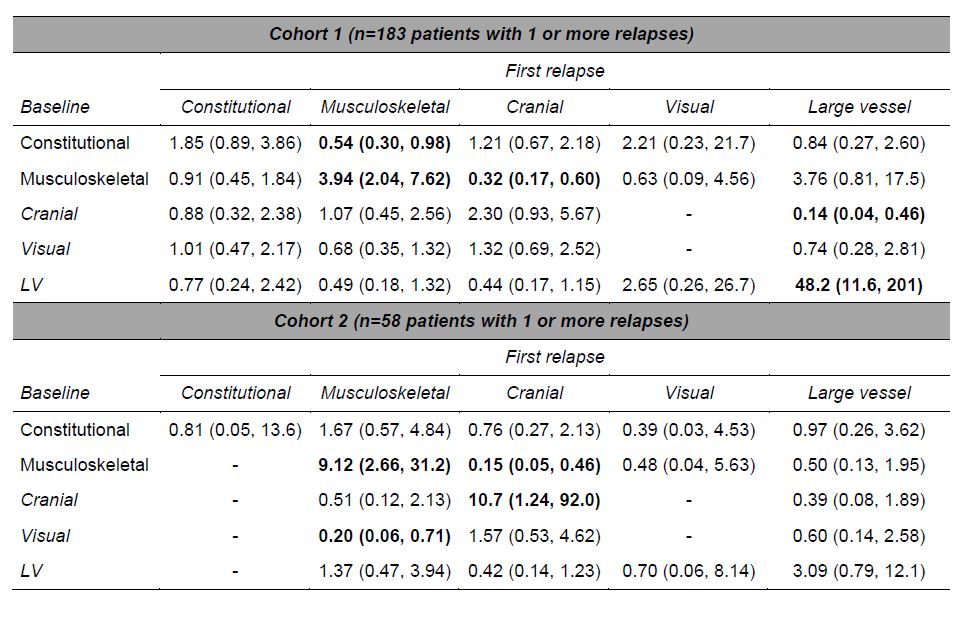
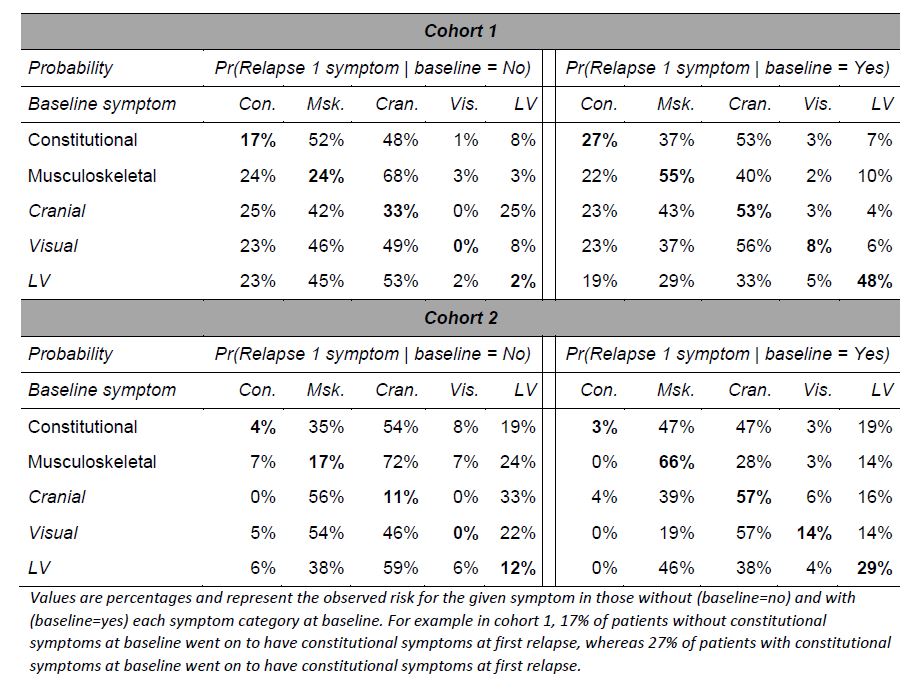
Results: In cohort 1 (C1), 183/286 (64%) patients had at least one relapse, whereas cohort 2 (C2) had 58/114 (51%) with at least one relapse. In C1, at first relapse 73% had symptoms in a single category, compared to 13% at baseline. At first relapse, 31% had cranial only, 30% MSK only, 9% constitutional only, 8% cranial plus constitutional, 7% cranial plus MSK. In C2, at first relapse 79% had symptoms in a single category, compared to 10% at baseline. At first relapse 33% had cranial only, 31% MSK only, 12% LV only, 9% cranial plus MSK. Odds ratios for presence of symptoms at first relapse based on presence of symptoms at baseline for C1 and C2 are shown in Table 1. In C1, patients with MSK symptoms at baseline were near 4 times more likely to have MSK features at first relapse but more than 3 times less likely to have cranial symptoms. Presence of LV symptoms at baseline resulted in a 48-fold increased odds of LV symptom at first relapse. In C2, patients with MSK at baseline had 9-fold greater odds of MSK at relapse but near 7-fold lower odds of cranial relapse symptoms. In C1, 21% and C2, 19% of patients went on to have new symptom categories at first relapse that were not present at baseline. Conditional probabilities of symptoms at first relapse according to presence or absence of baseline symptoms are shown in Table 2. No patient without visual symptoms at baseline developed visual symptoms at first relapse in either cohort. At first relapse new constitutional symptoms (17% C1, 4% C2), MSK (24% C1, 17% C2), cranial (33% C1, 11% C2), LV (2% C1, 12% C2) features were seen among patients that did not have these at baseline.
Conclusion: Relapse in GCA is common. Patients with MSK features at onset have greater odds of MSK but lower odds of cranial symptoms at relapse. New GCA symptoms not present at baseline occur in approximately 20% of first relapses, therefore providers should educate patients on the spectrum of GCA symptoms to be aware of, even beyond those present at a patient’s diagnosis.
To cite this abstract in AMA style:
Guarda M, Hanson A, Langenfeld H, Crowson C, Rakholiya J, Labarca C, Weyand C, Warrington K, Koster M. Concordance of Relapse Symptoms with Initial Baseline Presentation Features Among Patients with Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/concordance-of-relapse-symptoms-with-initial-baseline-presentation-features-among-patients-with-giant-cell-arteritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/concordance-of-relapse-symptoms-with-initial-baseline-presentation-features-among-patients-with-giant-cell-arteritis/