Session Information
Date: Tuesday, November 12, 2019
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster III: Giant Cell Arteritis
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Diagnostic assessment in giant cell arteritis (GCA) is rapidly changing as large-vessel (LV) involvement becomes increasingly recognized and non-invasive vascular imaging techniques become more available. The purpose of this study was to assess how clinicians around the world use diagnostic assessment strategies to assess arterial involvement in GCA.
Methods: Patients were included from a large, international cohort with standardized data collection from 2011-2017. Study centers were located in Asia, Australia/New Zealand, Europe, and North America. All patients had a confirmed diagnosis of GCA. Diagnostic assessments were performed at the discretion of the submitting physician. LV-imaging included angiography, ultrasonography, or PET imaging of the extra-cranial arteries. Temporal artery assessment included temporal artery biopsy (TAB) or ultrasonography (TA-US). Nominal logistic regression was used to study the associations between the decision to obtain a TAB and demographic data, ischemic cranial symptoms, and large-vessel involvement (aorta and its primary branches).
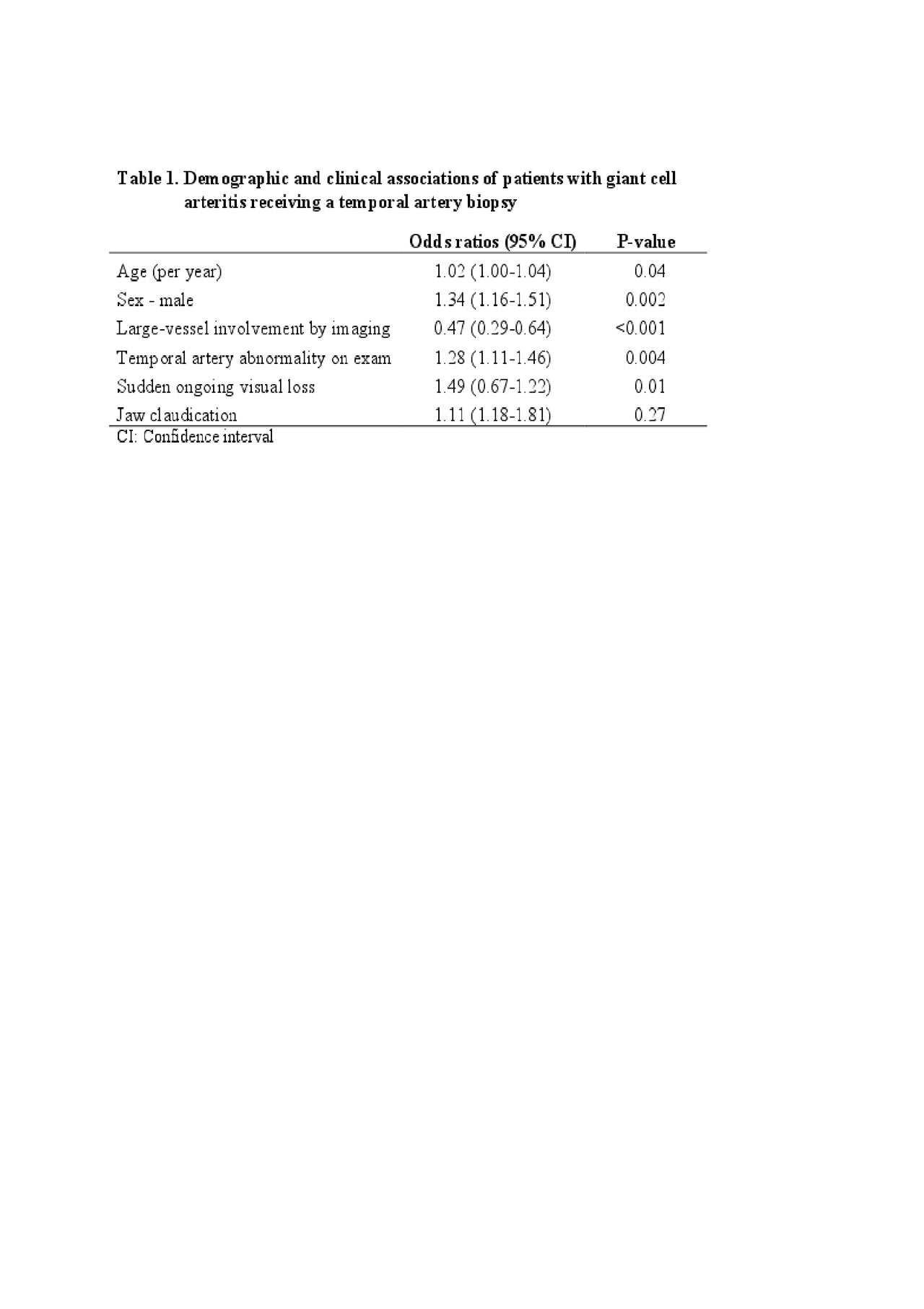
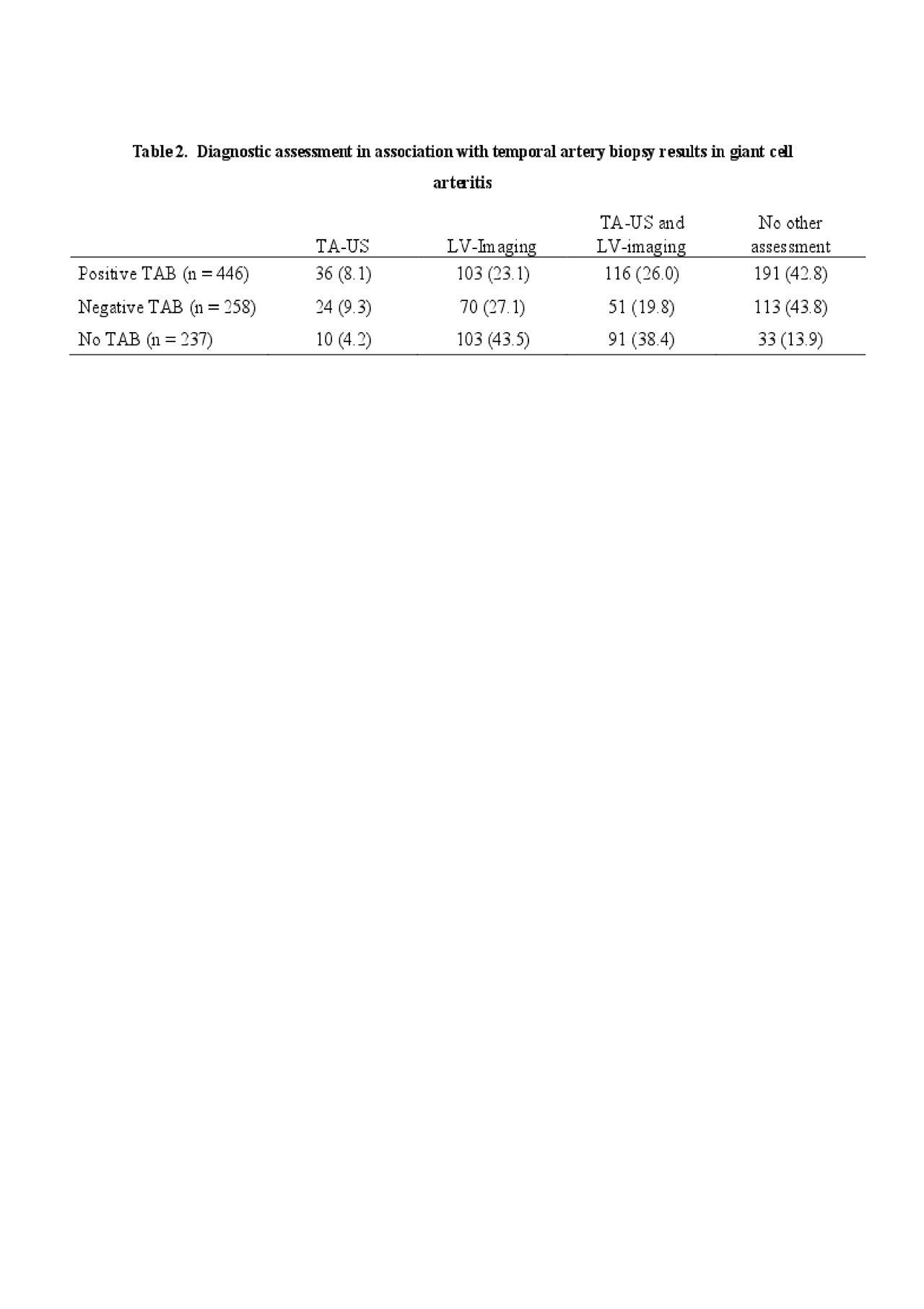
Results: 941 patients with GCA from 72 centers were included in the analysis, 783 (83%) patients were Europe, 111 (12%) patients from North America, and 47 (5%) patients from other regions. Overall, 704 patients (75%) had a TAB, 446 TABs (66%) were considered diagnostic for GCA. 328 (35%) patients had a TA-US, 258 (79%) patients had a halo sign and most came from European centers (n=321, 98%). 534 patients (57%) had LV-imaging, 40% (n=216) showed LV involvement. 431 patients (45%) had both LV-imaging and temporal artery-assessment. Only 33 patients (4%) did not have any diagnostic testing performed beyond clinical assessment. Male patients were significantly more likely to undergo a TAB than female patients, independent of cranial ischemic symptoms, age at diagnosis, temporal-artery abnormality on physician exam, or presence of LV involvement (Table 1). There was no sex preference in the rate of TA-US (Male: 37% vs Female: 34%, p=0.38) or LV-imaging (Male: 58% vs Female: 56%, p=0.70). Patients who received a TAB were older (mean age 73 years vs 71 years, p< 0.01) and patients who received LV-imaging were younger (mean age 72 years vs 74 years, p< 0.01). Most patients had multiple forms of diagnostic assessment (Table 2). Regardless of TAB results, approximately 60% of patients had vascular imaging studies performed in addition to biopsy. Vascular imaging was performed in 86% of patients who did not have a TAB and confirmed disease in 70% of these patients. TA-US was rarely used alone as a form of assessment. 69% (n=227) of patients with a TA-US also underwent TAB. Only 1% of patients had TA-US without another form of assessment compared to the 11% and 32% of patients that had only LV-imaging and TAB.
Conclusion: Vascular imaging is increasingly incorporated into the diagnostic assessment of GCA. The majority of patients with GCA underwent multiple forms of diagnostic testing, including TAB and vascular imaging studies. Demographic factors, clinical features, and regional differences in clinical practice influence diagnostic assessment strategies in GCA.
To cite this abstract in AMA style:
Gribbons K, Ponte C, Craven A, Robson J, Suppiah R, Luqmani R, Watts R, Merkel P, Grayson P. Comparisons of Strategies for Diagnostic Assessment in Giant Cell Arteritis: Results from an International Observational Cohort [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/comparisons-of-strategies-for-diagnostic-assessment-in-giant-cell-arteritis-results-from-an-international-observational-cohort/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparisons-of-strategies-for-diagnostic-assessment-in-giant-cell-arteritis-results-from-an-international-observational-cohort/