Session Information
Date: Monday, November 9, 2015
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: We aimed to compare patient reported
outcomes between adults with juvenile idiopathic arthritis (JIA) and adults
with rheumatoid arthritis (RA) with similar disease duration and treatment era.
Methods: This cross sectional study used a random
observation from JIA and RA participants in the National Data Bank for
Rheumatic Diseases (NDB), a longitudinal cohort of patients that complete
biannual questionnaires. Participants were included in the JIA group if they
were <55 years old at enrollment and had a physician diagnosis of JIA, a self-diagnosis
of JIA (with a physician diagnosis of arthritis), or a physician diagnosis of
RA with symptoms prior to age 16. Each JIA patient was matched to 3 RA patients
based on sex, calendar year of observation, and calendar year of diagnosis.
This produced matching disease duration and treatment era while minimizing
effects of comorbid conditions unrelated to arthritis. The demographics, patient
reported outcomes, and disease characteristics were compared between the JIA
and RA groups using Chi square or t tests. The SF-36 physical and mental
component summary scores, the patient activity score (PAS), and PAS-II were
compared between groups using stepwise reduced linear regression models.
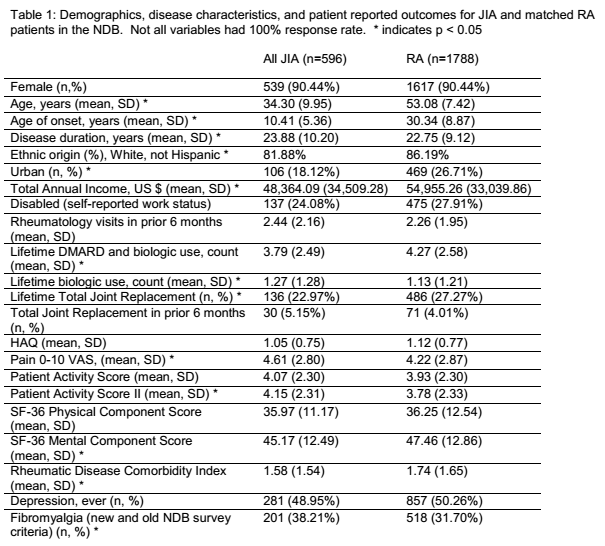
Results: We identified 596 JIA patients who were matched to
1788 RA patients; 90% were female. The JIA patients had a mean (SD) age of 34.3
years (10.0) and 82% were white; the RA patients had a mean age 53.1 (7.4) and
86% were white. Patients with RA were more likely to have a history of total
joint replacement, cancer, heart disease, liver disease, or cataract and have a
higher rheumatic disease comorbidity index. Patients with JIA report higher
pain scores, longer morning stiffness, have a higher PAS and PAS-II, and lower
SF-36 MCS (Table 1). After including 18 potential confounders, JIA diagnosis was
not significantly associated with the SF-36 PCS (beta 0.39, 95% CI -0.70, 1.49),
MCS (beta 0.06, 95% CI -1.73, 1.86), PAS (beta -0.06, 95% CI -0.26, 0.13), or
PAS-II (beta 0.09, 95% CI -0.12, 0.31). Each final model included 8-12
variables; variables with significant associations in all 4 models were the
number of rheumatology visits in the prior 6 months, meeting fibromyalgia
criteria, household income, having a total joint replacement in the prior 6
months, the rheumatic disease comorbidity index, and the cumulative number of
biologic medications.
Conclusion: JIA patients have different disease
characteristics and patient reported outcomes compared to RA patients matched on
disease duration and treatment era. JIA patients had active disease in
adulthood with similar number of visits to rheumatology and higher pain scores
than RA patients. Comorbidities, disease severity, and fibromyalgia may explain
the lower SF-36 MCS and higher PAS-II among JIA patients rather than age of
diagnosis. This is the first study to compare patient reported outcomes of
adult JIA patients to RA patients.
To cite this abstract in AMA style:
Mannion ML, Pedro S, Beukelman T, Curtis JR, Michaud K. Comparison of JIA and RA Patients in the National Data Bank for Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/comparison-of-jia-and-ra-patients-in-the-national-data-bank-for-rheumatic-diseases/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparison-of-jia-and-ra-patients-in-the-national-data-bank-for-rheumatic-diseases/