Session Information
Date: Monday, November 6, 2017
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: RA is estimated to affect approximately 1.3 million adults in the US and accounts for a significant proportion of US health care spend with direct medical costs of over $70 billion a year. The primary driver of cost in RA are the specialty drug classes. Given the cost differential between available RA treatments, it is critical to ensure that patients are receiving optimal therapy at the optimal time. We compared improvements in disease activity between biologic DMARD classes, in a large cohort of patients with RA, under conditions of routine clinical practice.
Methods: The OM1 platform collects, links, and leverages, structured and unstructured data from electronic medical records (EMR) and other sources in an ongoing and continuously updating manner. The OM1 RA Cohort includes data on >75,000 patients treated by rheumatologists. Disease activity measures (measured and identified using advanced natural language processing) were available in 59,326 patients and established American College of Rheumatology cutpoints were used to define disease severity. There were an average of 9.1 (imputed + observed) disease activity measures per patient. The analysis included patients who were treated with the same biologic disease modifying anti-rheumatic drug (bDMARD) for a 6-month period and had disease activity measures at baseline and at 6 months.
Results: The mean±SD age was 60±14 years, 76% of the cohort was female, and 71% Caucasian.
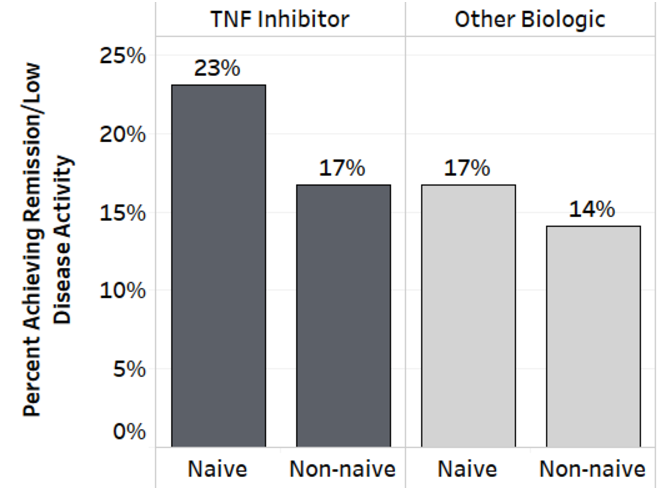
At baseline, 23% of patients were in remission, and 36%, 24% and 17% had low, moderate and high disease activity, respectively. Total and swollen joint counts were available in ~40% of the cohort and erythrocyte sedimentation rate was available in 70%. During the study period, 44% of the cohort received nonbiologic DMARD and 45% bDMARD; tumor necrosis factor inhibitor (TNF-inhibitor) accounted for 77% of bDMARD. The figure presents proportion of patients treated with bDMARD (categorized as TNF-inhibitor, n=9,574, 18% [95% CI: 17%-18%], and other bDMARD, n=5,877, 14% [13%-15%] for naive and non-naive patients combined), with moderate to severe disease at baseline, who achieved low or remission status within the subsequent 6 months. Analysis was stratified by whether they had documented prior treatment with biologics.
Conclusion:
Using a data driven platform that enables large scale assessment (patient characteristics, treatment patterns, clinical outcomes) of patients, we found that naive patients treated with TNF-inhibitors showed the most improvement in disease activity overall. Among non-naive patients the TNF-inhibitor group had the highest proportion of patients achieving remission or low disease activity over a 6-month treatment period.
To cite this abstract in AMA style:
Gliklich R, Su Z, Donadio G, Brecht T, Boussios C, O’Donovan F, Kekeh C, Lafontant A, Starzyk K, Menon V. Comparison of Improvements in Disease Activity between Classes of Biologic Disease Modifying Anti-Rheumatic Drugs in Routine Clinical Practice: Findings from a Large Contemporaneous Real World Cohort [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/comparison-of-improvements-in-disease-activity-between-classes-of-biologic-disease-modifying-anti-rheumatic-drugs-in-routine-clinical-practice-findings-from-a-large-contemporaneous-real-world-cohort/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparison-of-improvements-in-disease-activity-between-classes-of-biologic-disease-modifying-anti-rheumatic-drugs-in-routine-clinical-practice-findings-from-a-large-contemporaneous-real-world-cohort/