Session Information
Session Type: ACR/ARHP Combined Abstract Session
Session Time: 9:00AM-11:00AM
Background/Purpose: Several studies have suggested that patients with elderly-onset rheumatoid arthritis (EORA) receive biologic treatments less frequently than patients with younger-onset RA (YORA). This has been demonstrated even in patients with comparable disease activity. Risk of treatment complications and financial challenges associated with Medicare reimbursement may also contribute to this disparity. Our objective was to compare biologic drug discontinuation rates for older vs. younger onset RA, as this is a key outcome measure that could impact prescribing practices.
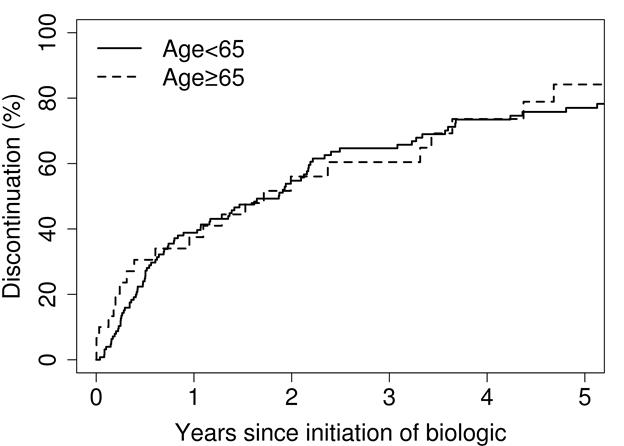
Methods: A retrospective medical record review was performed of all patients who fulfilled the 1987 ACR criteria for adult-onset RA in 1980-2013 among residents of a geographically defined area with follow up until death, migration or July 1, 2016. EORA was defined as RA diagnosis at age ≥ 65 years and YORA was defined as age 18-64 years. Discontinuation rates were estimated using cumulative incidence adjusted for the competing risk of death. Risk factors were examined using Cox models adjusted for age, sex and calendar year of RA incidence.
Results: 171 cases of EORA and 435 cases of YORA were identified (67% and 71% female respectively, p=0.33). EORA patients had a lower rate smoking at time of RA diagnosis (8% vs. 18%, p=0.002), though ever smoking was not a significant risk factor for starting a biologic (p=0.42). There were no significant differences in rheumatoid factor (RF) or anti-cyclic citrullinated peptide antibody (CCP) positivity (p=0.26) or body mass index (BMI) (p=0.23) at time of diagnosis. Cumulative incidence of biologic initiation was lower among EORA compared with YORA (11% vs 19% at 2 year after RA diagnosis, respectively, p<0.001). Among those treated with a biologic, years from RA diagnosis to first biologic was not significantly different between the two groups (p=0.17). Cumulative incidence of first biologic discontinuation was 38% at 1 year (95% confidence interval [CI], 23-61%) and 56% at 2 years (95% CI, 40-79%) for EORA compared with 39% at 1 year (95% CI, 31-49%) and 55% at 2 years (95% CI, 46-65%) for YORA (p=0.61). Concurrent glucocorticoid use at initiation of first biologic was statistically significantly associated with a lower risk for discontinuation in EORA (hazard ratio: 0.19; 95% confidence interval: 0.06-0.59), but not in YORA (interaction p=0.06). There were no significant predictive factors for discontinuation in YORA.
Conclusion: Discontinuation rates of biologic medications did not differ significantly between patients with EORA and YORA.
To cite this abstract in AMA style:
Richter M, Matteson EL, Davis JM III, Achenbach SJ, Crowson CS. Comparison of Biologic Discontinuation in Patients with Elderly-Onset Vs Younger-Onset Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/comparison-of-biologic-discontinuation-in-patients-with-elderly-onset-vs-younger-onset-rheumatoid-arthritis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparison-of-biologic-discontinuation-in-patients-with-elderly-onset-vs-younger-onset-rheumatoid-arthritis/