Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Cardiovascular (CV) risk estimation across diverse rheumatoid arthritis (RA) cohorts may be challenging given potential heterogeneity in comorbidities and widely varying prevalence of CV risk factors. The generalizability of CV risk among younger disabled RA patients enrolled in the Medicare program to similarly-aged patients who are commercially insured is unclear. We aimed to compare CV rates in Medicare and Marketscan to assess comparability.
Methods: Three cohorts of rheumatoid arthritis (RA) patients 40≤ age < 65 years were created using 2006-2016 Medicare and Marketscan claims data respectively. In each dataset, Cohort 1 was defined as ≥2 diagnosis codes for RA occurring 7 -365 days apart with ≥1 diagnosis code from a rheumatologist; Cohort 2 was defined as ≥1 diagnosis code for RA from rheumatologist followed by use of disease-modifying antirheumatic drugs (DMARDS, conventional, biologic or small molecule); Cohort 3 was defined as Cohort 2, plus initiation of a new biologic/tofacitinib, used as a proxy for greater RA disease activity. Other autoimmune diseases, malignancy, past myocardial infarction (MI), or stroke were exclusionary.
Follow up started at the earliest date of meeting the cohort definition and the requirement of one year of medical and pharmacy coverage and ended at earliest of: 1) a CV outcome (hospitalized MI or stroke, using validated algorithms); 2) end of enrollment 3) age 65 years; 4) end of biologic exposure plus 90 days (cohort 3 only).
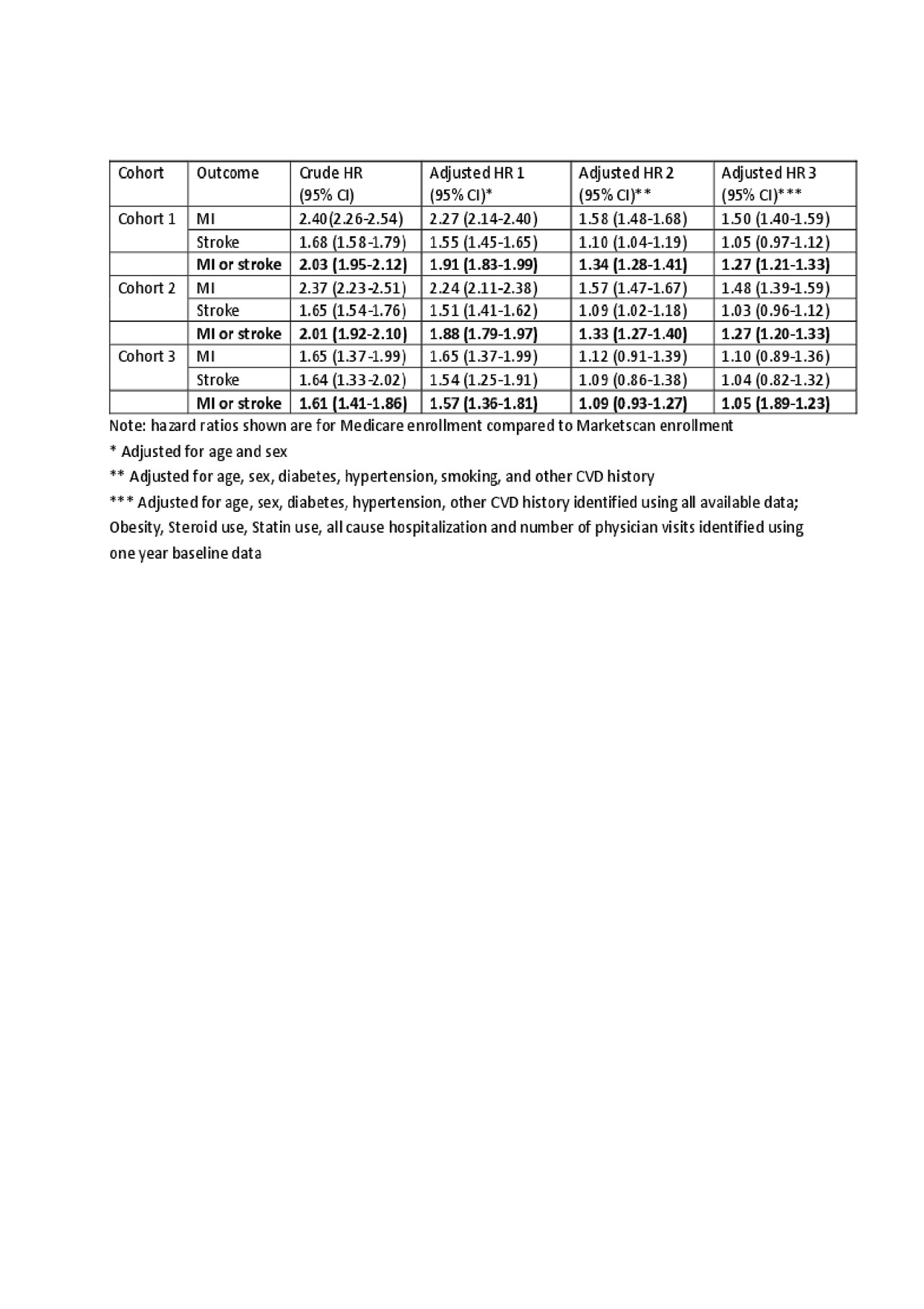
Descriptive statistics including standardized mean differences (SMDs) and CV incidence rates (IR) were calculated, and Poisson regression used to generate confidence intervals (CI). Cox regression was used to generate hazard ratio (HR), comparing enrollment in Medicare vs. Marketscan. Models sequentially adjusted for age and sex (model 1); model 1 + diabetes, smoking, hypertension, high CV risk (model 2): and model 2 + a variety of additional risk factors (model 3).
Results: A total of 380,336 RA patients comprised cohort 1 (mean age 53.3 (SD 8.1) years for Medicare and 51.1 (SD 8.8) years for Market Scan, and 21-23% were male). All co-morbidities and medication use were more prevalent in Medicare than Marketscan. Age- and sex-specific IRs were approximately 1.5-2.5-fold greater in Medicare referent to Marketscan. After intermediate adjustment (model 2), RA patients in Medicare in cohort 2 still had higher CV risk (adjusted HR 1.33, 95% CI 1.27-1.40). However, cohort 3 requirements attenuated MI and stroke risk to be negligibly different between Medicare and Marketscan RA patients (adjusted HR 1.09, 95% CI 0.93-1.27).
Conclusion: The rate of CV events varies substantially between different RA cohorts, but multivariable adjustment and careful attention to RA-related features including medication initiation (used as a proxy to reduce heterogeneity in disease activity) can minimize these differences.

table 1 ACR abstract–Comparing CVD in Medicare and MarketScan v3_fx
ACR abstract–Comparing CVD in Medicare and MarketScan v3_fx 3
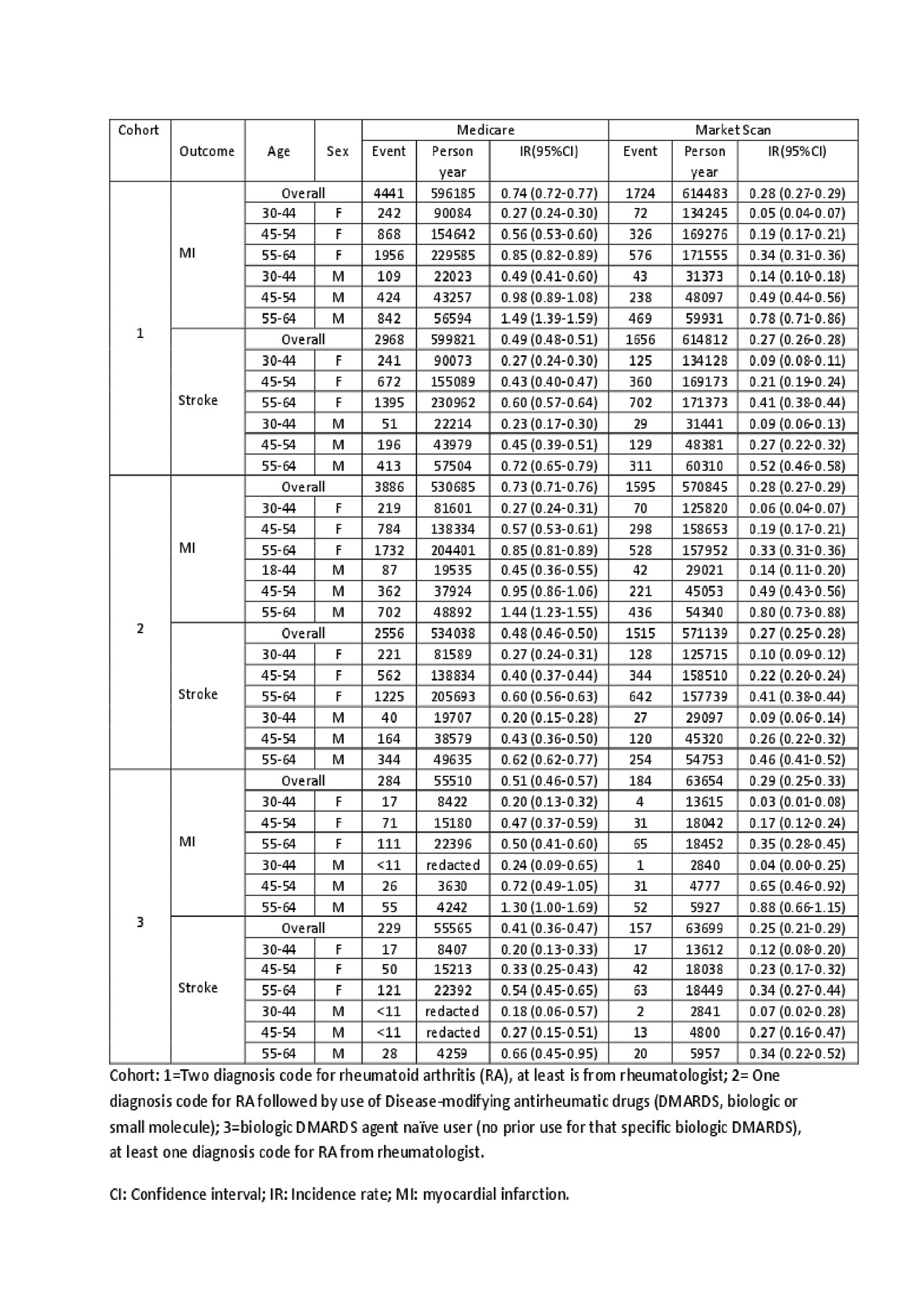
table 2b ACR abstract–Comparing CVD in Medicare and MarketScan v3_fx
To cite this abstract in AMA style:
Xie F, Crowson C, Navarro-Millan I, Safford M, Curtis J. Comparing the Generalizability of Cardiovascular Risk in Different Rheumatoid Arthritis Cohorts [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/comparing-the-generalizability-of-cardiovascular-risk-in-different-rheumatoid-arthritis-cohorts/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparing-the-generalizability-of-cardiovascular-risk-in-different-rheumatoid-arthritis-cohorts/
