Session Information
Date: Tuesday, November 14, 2023
Title: (1996–2018) Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science Poster
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Although clinical trials have shown that denosumab (Dmab) significantly increases bone mineral density at key skeletal sites more than oral bisphosphonates, evidence is lacking from head-to-head randomized trials evaluating fracture outcomes. This retrospective observational study evaluated the comparative effectiveness of Dmab versus alendronate (Aln) in reducing fracture risk among postmenopausal women with osteoporosis (PMO) in the U.S.
Methods: Female Medicare fee-for-service beneficiaries ≥ 66 years of age who newly initiated Dmab (n=89,115) or Aln (n=389,536) between January 1, 2012 to December 31, 2018 with no prior history of osteoporosis treatment, were followed from treatment initiation until the first instance of a specific fracture outcome, treatment discontinuation (defined as the end of treatment supply + 60-day allowable gap) or switch, Medicare disenrollment, death, or end of available data (December 31, 2019). A doubly robust inverse-probability of treatment (weights estimated from multivariate logistic regression models) and censoring (weights estimated from multivariate Cox Proportional Hazards regression models) weighted function was used to estimate the relative risk (RR) associated with the use of Dmab compared with Aln for hip, nonvertebral (NV; includes hip, humerus, pelvis, radius/ulna, other femur), non-hip, nonvertebral (NHNV), hospitalized vertebral (HV), and major osteoporotic (MOP; nonvertebral and hospitalized vertebral) fractures.
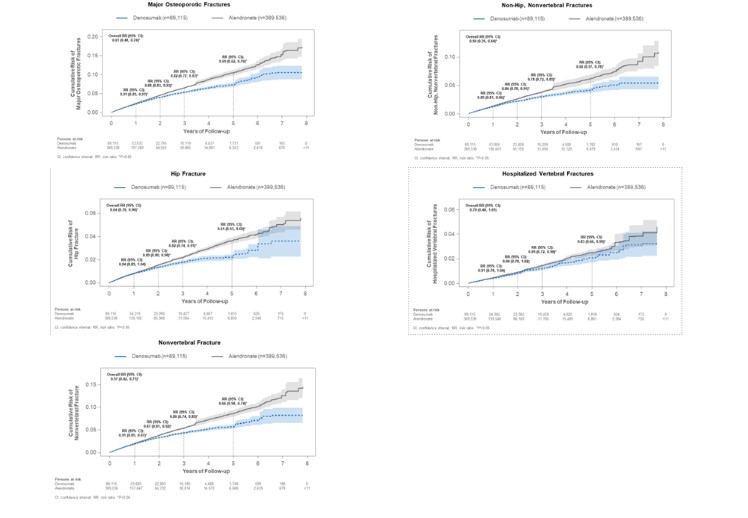
Results: Overall, Dmab reduced the risk of MOP by 39% (RR=0.61; 95% CI: 0.48-0.74), hip by 36% (0.64; 0.39-0.90), NV by 43% (0.57; 0.42-0.71), NHNV by 50% (0.50; 0.35-0.64), and HV fractures by 30% (0.70; 0.40-1.01) compared with Aln. Dmab reduced the risk of MOP fractures by 9% (0.91; 0.85-0.97) at year 1, 12% (0.88; 0.83-0.93) at year 2, 18% (0.82; 0.77-0.87) at year 3, and 31% (0.69; 0.62-0.76) at year 5.An increase in the magnitude of fracture risk reduction with increasing duration of exposure was also observed for other NV outcomes(Figure).
Conclusion: In a cohort of almost a half million, treatment-naive PMO, we observed robust and significant reductions in the risk of MOP, hip, NV, NHNV, and HV fractures for patients on Dmab compared to Aln. Patients who remained on Dmab for longer periods of time experienced greater reductions in fracture risk.
To cite this abstract in AMA style:
Curtis J, Arora T, Liu Y, Lin T, Spangler L, Brunetti V, Stad R, McDermott M, Bradbury B, Kim M. Comparative Effectiveness of Denosumab versus Alendronate Among Postmenopausal Women with Osteoporosis in the U.S. Medicare Program [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/comparative-effectiveness-of-denosumab-versus-alendronate-among-postmenopausal-women-with-osteoporosis-in-the-u-s-medicare-program/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparative-effectiveness-of-denosumab-versus-alendronate-among-postmenopausal-women-with-osteoporosis-in-the-u-s-medicare-program/