Session Information
Session Type: ACR Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Anti-neutrophil cytoplasmic antibodies (ANCA) have been identified in patients who have pneumonia without a diagnosis of ANCA-associated vasculitis (AAV). These patients are presently categorized as having idiopathic pulmonary fibrosis (IPF). Recent criteria categorize patients with features of autoimmunity but without a defined connective tissue disease as having interstitial pneumonitis with autoimmune features (IPAF). However, these criteria do not include ANCA. Growing evidence suggests that patients with ILD and ANCA may present differently from those with ILD in the setting of AAV or IPF.
Methods: We performed a retrospective case-cohort study of ANCA-associated ILD and randomly selected age and gender-matched controls with IPAF. Both groups were followed at the University of Chicago (1/2005 – 10/2018). Data on autoimmune serologies, baseline high-resolution CT scan using CALIPER (Computer-Aided Lung Informatics for Pathology Evaluation and Rating) parameters, baseline and longitudinal pulmonary functional tests (PFTs), vital status and lung transplant were collected from the electronic medical records. Variable comparisons utilized the Student’s t-test or chi-squared, while panel data was evaluated with mixed-effect modeling. Survival analysis was computed using Cox regression models and the Kaplan-Meier estimator. (IRB#18-03349; #14163-A).
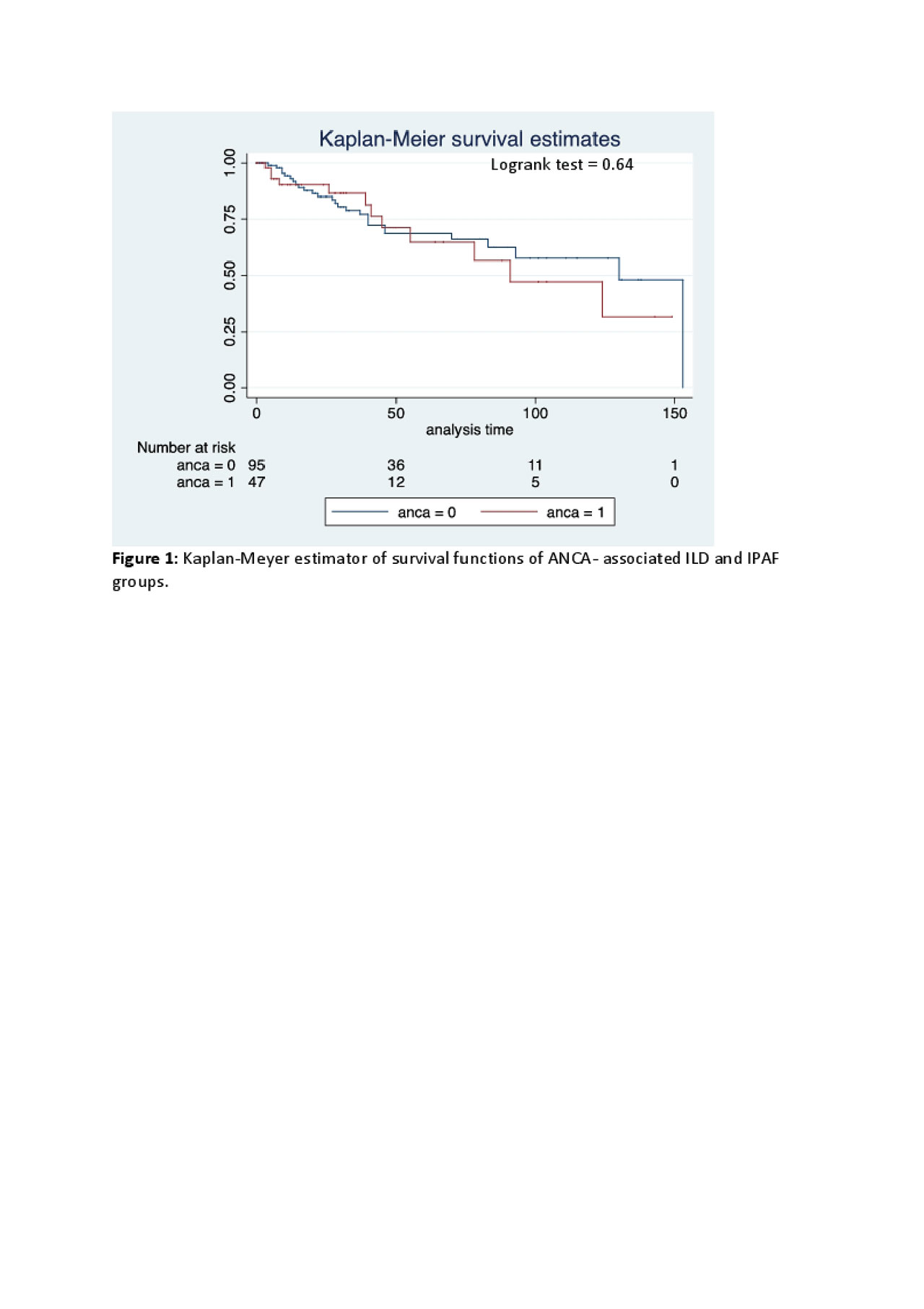
Results: In the study population (ANCA-associated ILD, n=52; IPAF, n=101), the mean age at ILD diagnosis was 63yrs, and 59% were women. Compared to white subjects, racial/ethnic minorities had lower TLC%, FVC%, FEV1%, and DLCO% (P=0.004, 0.003, 0.011, and 0.08 respectively). Groups were otherwise comparable with respect to race (Table 1). The prevalence of other autoimmune antibodies appeared greater in ANCA-associated ILD compared to IPAF, however these differences were not statistically significant (Table 1). Baseline and longitudinal PFTs were similar between both groups. Patients with ANCA-associated ILD had greater honeycombing in central portions of the lower lobes, and the central region of the left middle lobe (Table 2). ANCA positivity was not predictive of mortality (Figure 1), whereas total lung vessel volume, older age, non-White race, and lower DLCO% (P=0.043, < 0.001, 0.008, 0.054 respectively) were associated with mortality.
Conclusion: This is the largest US study comparing ANCA-associated ILD to IPAF. Our results suggest that these groups are similar, and these findings may argue in favor of adding ANCA to the IPAF criteria. Our radiographic data also suggests that ANCA-associated ILD may be driven by inhaled antigens and airway inflammation, leading to centrilobular fibrosis.
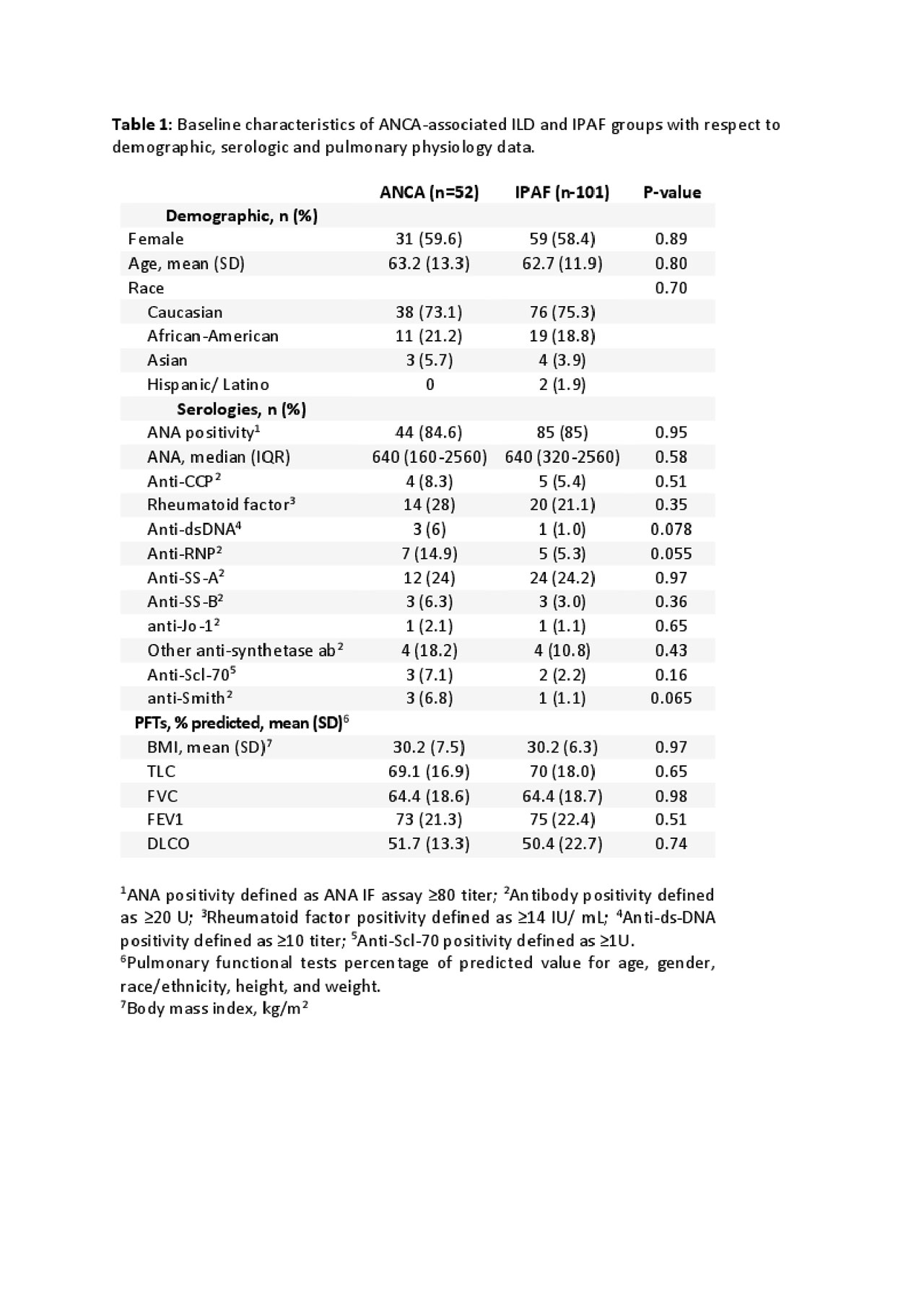
Table 1 – Demographic -serology – PFTS
To cite this abstract in AMA style:
Ventura I, Dua A, Adegunsoye A, Strek M, Curran J, Weiss A, Chung J. Comparative Analysis Between ANCA-associated Interstitial Lung Disease and Interstitial Pneumonitis with Autoimmune Features [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/comparative-analysis-between-anca-associated-interstitial-lung-disease-and-interstitial-pneumonitis-with-autoimmune-features/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/comparative-analysis-between-anca-associated-interstitial-lung-disease-and-interstitial-pneumonitis-with-autoimmune-features/