Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
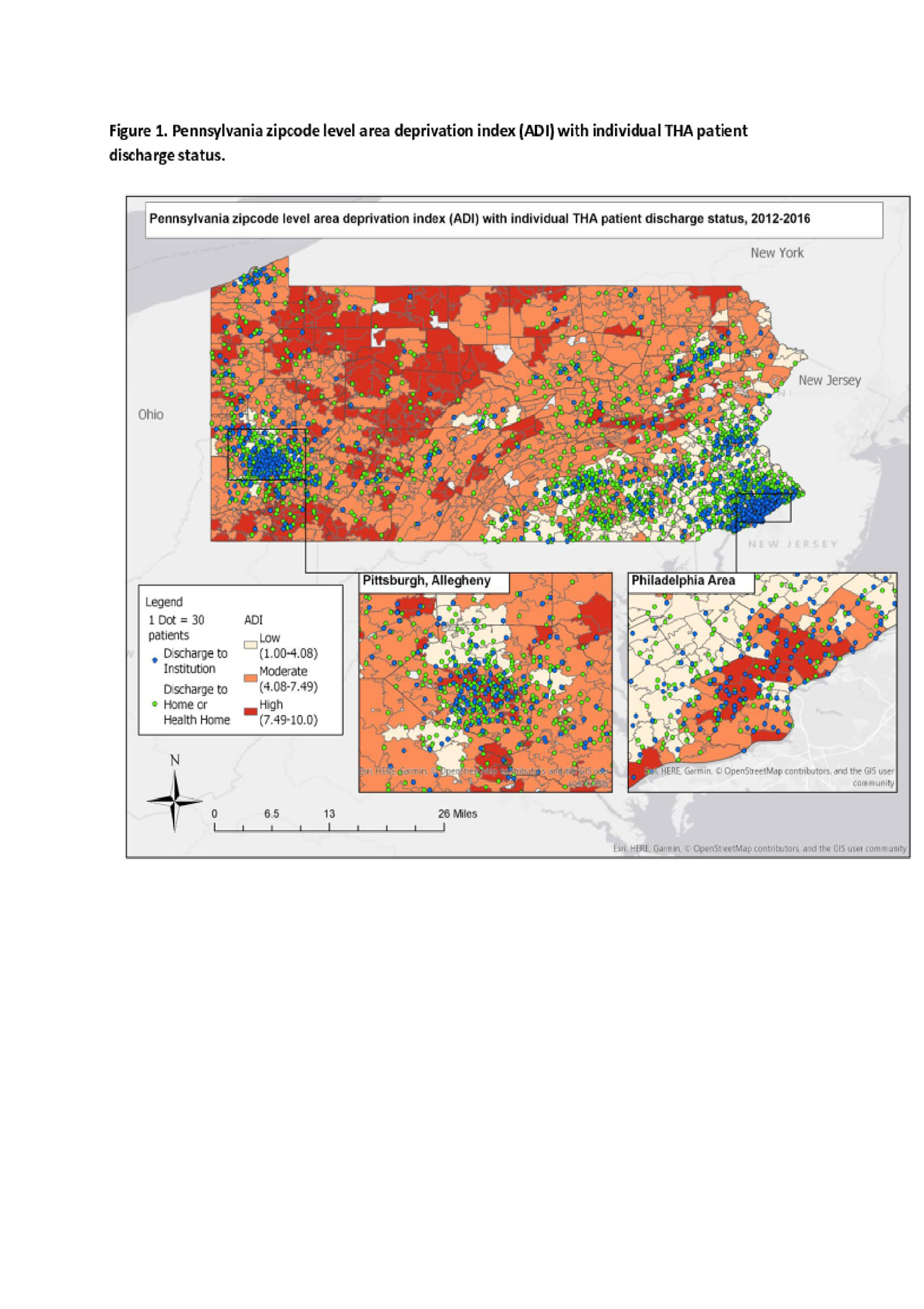
Background/Purpose: With the aging of the world population and the rising prevalence of Hip Osteoarthritis (OA), elective total hip arthroplasty (THA) has become one of the fastest growing procedures in the management of end-stage OA. Medicare, the largest payer in the US of joint replacement surgery, has introduced several payment reform models that target discharge destination and risk of readmission. In additional to clinical factors, social factors such as where one lives that might impact where patients go for post-op care and rehab following elective total hip replacement surgery.We sought to examine how the socioeconomic status of the community in which one lives influences discharge disposition and the odds of 90-day readmission after elective THA.
Methods: We used the Pennsylvania Health Care Cost Containment Council (PHC4) database to identify all patients who underwent elective THA between 2012 and 2016. We also derived Community level Area Deprivation Index (ADI) from the American Census Survey. We used binary logistic regression models to test the association between community ADI and the discharge outcome of Institution vs. Home. We also modeled the risk of 90-day readmission for patients sent to an institution compared to home for post-op care and rehab. We adjusted for important clinical, demographic, and facility level covariates. To evaluate whether patient race affects this relationship, we included into the models an interaction term for community ADI and patient race.
Results: Our analytic sample consisted of 84, 931 who underwent THA between 2012 and 2016 within the State of Pennsylvania. The study sample is stratified by < 65 (n = 40, 304) and ≥ 65 (n = 44, 627) years of age groups. In the years < 65 group, 17.1 % came from high ADI communities (above Q3), 46.5% from middle strata ADI (within Q2 and Q3) and 36.4% from low ADI communities (below Q2). The distribution for high, middle, and low ADI among patients ≥ 65 years of age were 13.8%, 47.1%, and 39.1%, respectively. Compared to low ADI community patients, patients from high ADI communities were more likely to be discharged to an institution compared to home (p < 0.001 in both age groups), after controlling for patient and facility level characteristics. The interaction effect of race and ADI on discharge destination was statistically significant in those ≥ 65 years of age (p < 0.05), but not in patients < 65 years. The association of ADI on 90-day readmission was not statistically significant. The interaction of ADI and race on 90-day readmission was also not statistically significant.
Conclusion: In this large sample of patients who underwent THA in the State of Pennsylvania, the level of deprivation of the community in the patient resides influences where patients go for post-op care and rehab after elective THA disposition.
b Variables are compared by ADI for each age group -years < 65, ≥ 65- using Pearson χ2 test or fisher’s exact test, as appropriate. Significance levels: * = p<0.05, ** =
p<0.01, *** = p<0.001.
c Clinical comorbidities were identified based on coding algorithms developed by Quan and colleagues -enhanced Elixhauser version-, using either the ICD-9-CM or the ICD
10 coding system, as appropriate. The Elixhauser co-morbidity index score is calculated based on the cumulative number of comorbidity conditions.
To cite this abstract in AMA style:
Mehta B, Goodman S, Ho K, Parks M, Ibrahim S. Community-level Deprivation Index: Impact on Discharge Destination After Elective Hip Replacement [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/community-level-deprivation-index-impact-on-discharge-destination-after-elective-hip-replacement/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/community-level-deprivation-index-impact-on-discharge-destination-after-elective-hip-replacement/