Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Azathioprine is a widely-used drug for the treatment of rheumatic diseases, inflammatory bowel disease, and for organ transplantation. However, treatment is often limited by serious adverse events, such as leukopenia. Our ability to predict azathioprine-associated leukopenia is limited to the evaluation of the enzyme thiopurine methyl transferase (TPMT), either by functional assays or by the identification of variants in the gene TPMT which encodes it. We hypothesize that a risk score composed of multiple clinical factors and variants in selected candidate genes—in addition to TPMT—could improve the prediction of azathioprine-associated leukopenia.
Methods: This is a case-control study that used de-identified records from BioVU, a clinical practice-based biobank at a tertiary medical center to identify 425 Caucasian patients who received prescriptions for azathioprine. Subjects with a leukocyte count of less than 4,000 WBC/µL while receiving prescriptions for azathioprine were classified as cases. Subjects receiving prescriptions for azathioprine who did not develop leukopenia were classified as controls.
We reviewed the clinical records, collected clinical variables (age, sex, weight, clinical indication for azathioprine use, concurrent prescription of other medications, and azathioprine daily dose) and genotyped 71 genetic candidates identified through literature and database review. Genotyping of 60 single nucleotide polymorphisms passed quality control. We built two scores using the coefficients from multivariate regressions; leukopenia was the dependent variable. The first model was a logistic regression including TMPT status, age, and sex. The second model included TPMT status, age, sex, additional clinical variables listed above, and genetic candidates. To avoid overfitting, we used ridge regression, which uses a standard cross-validated penalty to shrink the coefficients of the covariates.
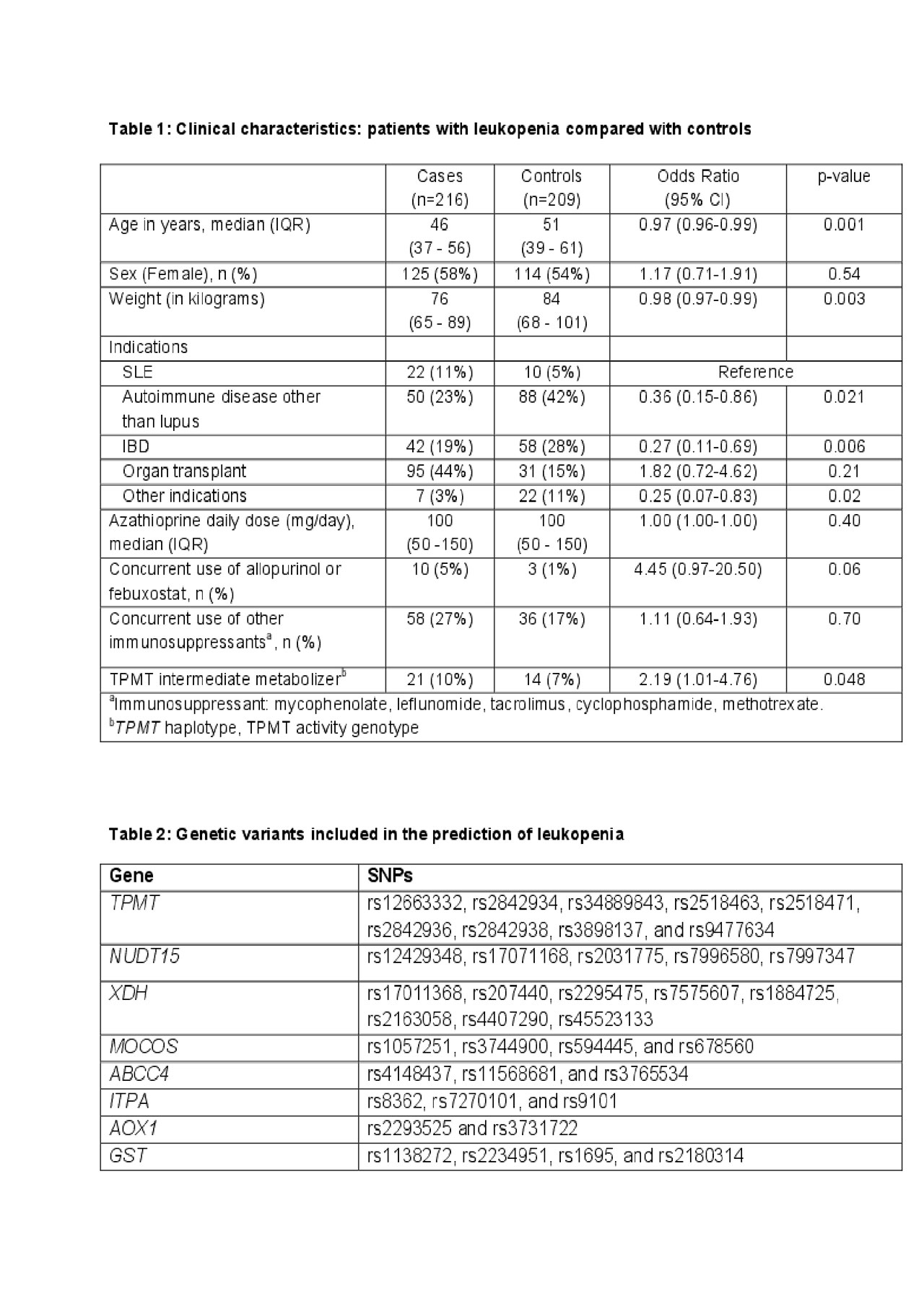
Results: 216 patients had azathioprine-associated leukopenia and 209 were control subjects. Younger age, lower weight, a diagnosis of systemic lupus erythematosus or organ transplant, and being a carrier of the TPMT haplotype corresponding to intermediate metabolizer status were significantly associated with leukopenia (Table 1). The area under the ROC curve (AUC) of a score based on a regression that included TPMT status, age, and sex was 0.59 (95% C.I.: 0.54-0.64). After shrinkage, the ridge model included 11 clinical and 47 genetic candidates (Table 2); the AUC of the score from that model increased to 0.77 (95% C.I.:0.73-0.82).
Conclusion: This proof-of-concept study investigates the utility of adding clinical and genetic variables to TMPT to improve discrimination of the risk for azathioprine-associated leukopenia. After shrinkage, we were able to show that a combined model, including clinical and genetic variants, improved our ability to predict leukopenia. Further studies in larger populations with independent replications are needed to further develop prediction scores that are useful for routine clinical practice.
To cite this abstract in AMA style:
Anandi P, Dickson A, Feng Q, Wei W, Dupont W, Plummer D, Liu G, Barker K, Kawai V, Birdwell K, Cox N, Stein C, Hung A, Chung C. Combining Clinical and Candidate Gene Data into a Risk Score for Azathioprine-Associated Leukopenia in Routine Clinical Practice [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/combining-clinical-and-candidate-gene-data-into-a-risk-score-for-azathioprine-associated-leukopenia-in-routine-clinical-practice/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/combining-clinical-and-candidate-gene-data-into-a-risk-score-for-azathioprine-associated-leukopenia-in-routine-clinical-practice/