Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Renal biopsy remains a cornerstone of management of lupus nephritis. Repeat renal biopsies after therapy help prognosticate renal outcomes. We sought to describe the histology of repeat renal biopsies in a cohort of lupus nephritis and determine the impact of change in histology on renal outcomes. We also studied the decline in glomerular filtration rate in those with repeat biopsied.
Methods: Out of 598 patients of SLE who were biopsied for suspected nephritis from 2001 to 2024, 95 underwent a second biopsy and 9 had a third biopsy. We reviewed the renal histology at each biopsy, class transitions and the estimated glomerular filtration rate (eGFR, 24 hour creatinine clearance). Outcomes studied were end stage renal disease (ESRD) and decline in eGFR. Paired Wilcoxon signed rank test was used to compare NIH activity, chronicity indices and eGFR at each biopsy.
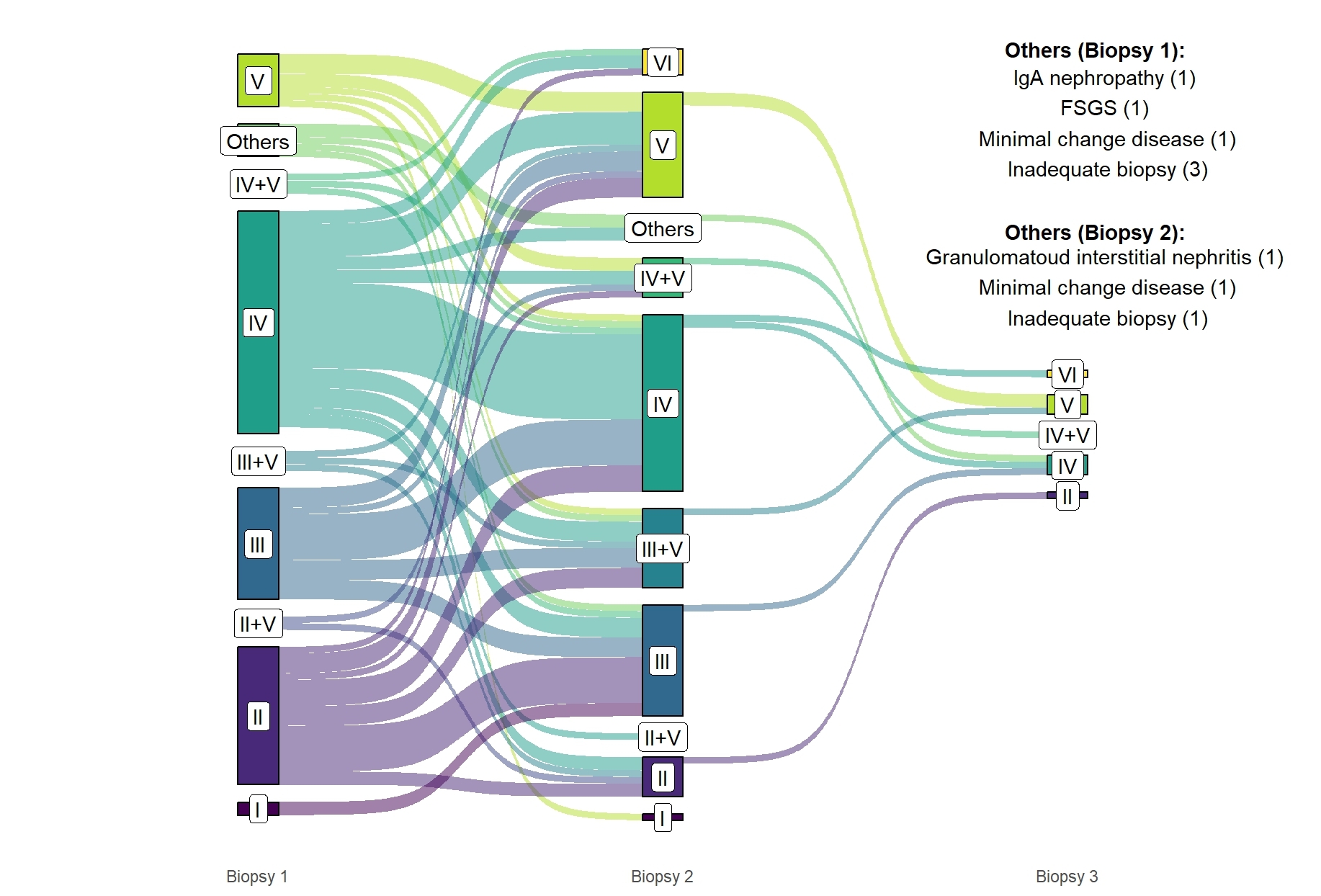
Results: The median time to first, second and third biopsies were 0.08 years (0.02-0.55), 6.32 years (2.91-9.56) and 11.66 years (7.83-14.48). On re-biopsy, class transitions occurred overall in 70 (73.68%) of the re-biopsied patients. However, these numbers differ in non-proliferative and proliferative nephritis. Transition from non-proliferative Class II and Class V nephritis at baseline to a proliferative form (Class III, IV or a combination of either and Class V) occurred in 16 (76.2%) and 4 (50%) of patients respectively. Transition from a proliferative Class III and Class IV nephritis at baseline to a non-proliferative form (Class I, II, V or a combination of II and V) occurred in 5 (25%) and 8 (21.6%) respectively. Transition to Class VI occurred in 4 patients at 2nd and 1 patient in 3rd biopsy from predominantly Class IV (4 patients) and Class II (1 patient) at baseline.
The NIH activity scores did not significantly differ between first (median 3, IQR 1-5), second (median 3, IQR 1-5) and third (median 3, IQR 2-5) biopsies. The NIH chronicity score rose significantly from first (median 1, IQR 0-2) to second biopsy (median 2.5, IQR 1-3.75) (P< 0.001) to third biopsy (median 5, IQR 3-8) (P< 0.05). The eGFR rose from first (median 33.5, IQR 22.5-53.8) to second biopsy (median 43.7, IQR 24.7-64) but then reduced markedly at the time of third biopsy (median 20.7, IQR7.7-30.1) (p< 0.05 for both).
Thirty-two (33.68%) of those with repeat biopsies developed ESRD. On multivariable logistic regression, a higher chronicity score at first biopsy (OR 1.99, 95% CI 1.05-3.77) was the only predictor of end stage renal disease on follow up. Class transitions did not affect the ultimate development of ESRD.
Conclusion: A high proportion of patients with non-proliferative nephritis, especially Class II nephritis transform to a proliferative class. These patients may warrant upfront treatment with potent immunosuppression. NIH Chronicity score progressively increases as damage accumulates. Higher chronicity scores at initial biopsy predict ESRD.
To cite this abstract in AMA style:
Chatterjee R, Vijayan N, Misra D, Agarwal V, Lawrence A, Aggarwal A. Clinical Utility of Repeat Renal Biopsies in Lupus Nephritis: The NIH Chronicity Index at First Biopsy Predicts Future End Stage Renal Disease in a Large South Asian Cohort of SLE [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/clinical-utility-of-repeat-renal-biopsies-in-lupus-nephritis-the-nih-chronicity-index-at-first-biopsy-predicts-future-end-stage-renal-disease-in-a-large-south-asian-cohort-of-sle/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-utility-of-repeat-renal-biopsies-in-lupus-nephritis-the-nih-chronicity-index-at-first-biopsy-predicts-future-end-stage-renal-disease-in-a-large-south-asian-cohort-of-sle/