Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Relapsing polychondritis (RP) is a systemic inflammatory disease that can be fatal. The main clinical feature that typically leads to diagnosis is ear inflammation, however the disease is very heterogeneous and can involve multiple organs. Failure to recognize RP can lead to diagnostic delay and further complications. The study objective was to identify specific phenotypes in a prospective cohort of patients with RP.
Methods: Patients 18 years and older were selected from a prospective, observational cohort. All patients met McAdams or Damiani’s diagnostic criteria for RP. Six clinical variables were used to identify clusters of patients using latent class analysis. Model selection was based on the akaike information criterion. Cases were assigned to a cluster based on probability of membership. The variables included in the model were saddle nose deformity, subglottic stenosis (SGS), tracheomalacia (TM), bronchomalacia (BM), ear inflammation and tenosynovitis/synovitis. SGS was defined as pathological narrowing of the subglottis visualized by laryngoscopy. TM was defined as antero-posterior and/or lateral flattening of the tracheal wall during expiration on dynamic CT of ≥50%. BM was defined as collapse of the bronchi during dynamic CT scan. Ear involvement was defined as physician-observed tender swelling of the pinna with associated redness. Differences were assessed by chi square or Kruskal-Wallis test. Median values are presented.
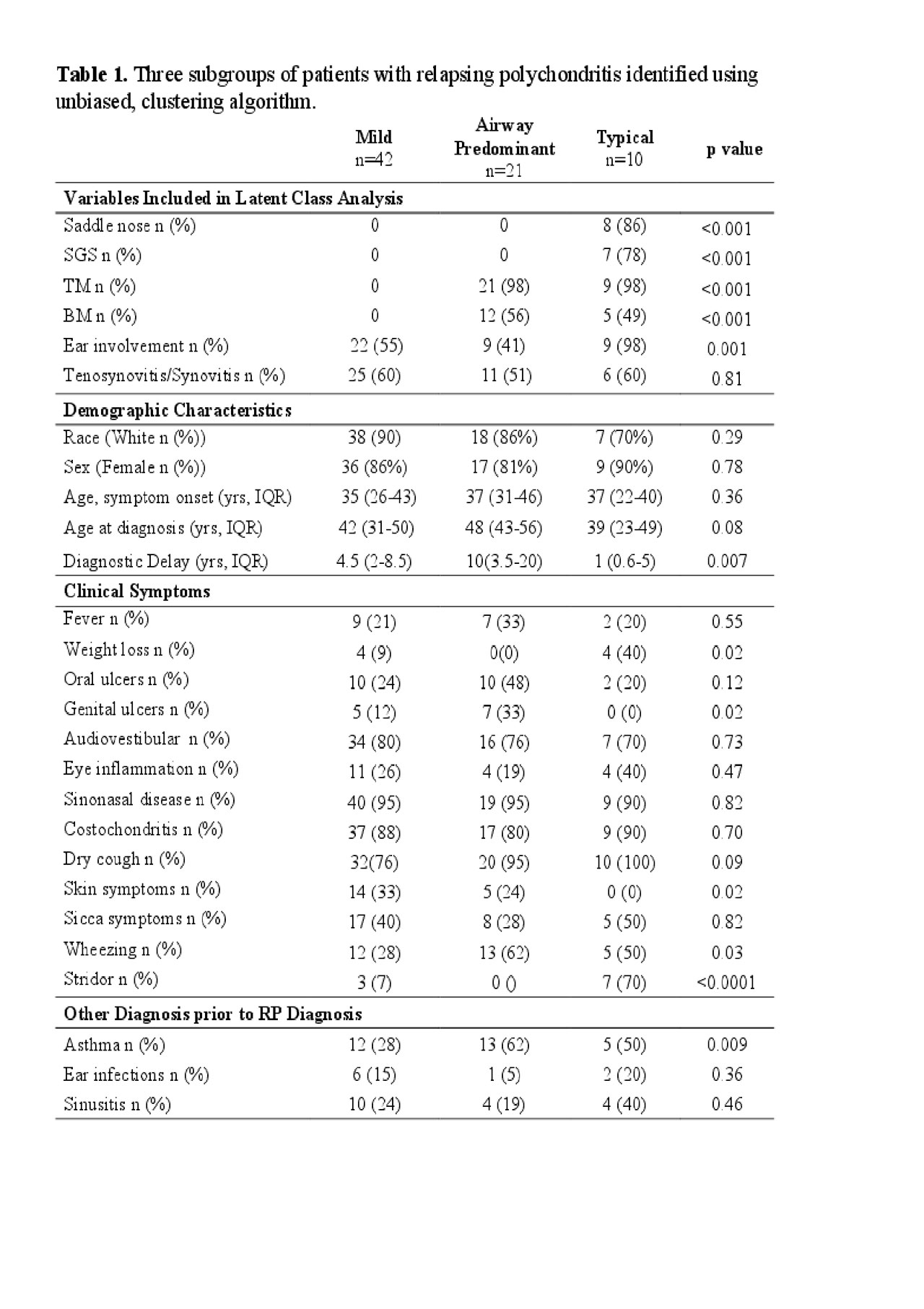
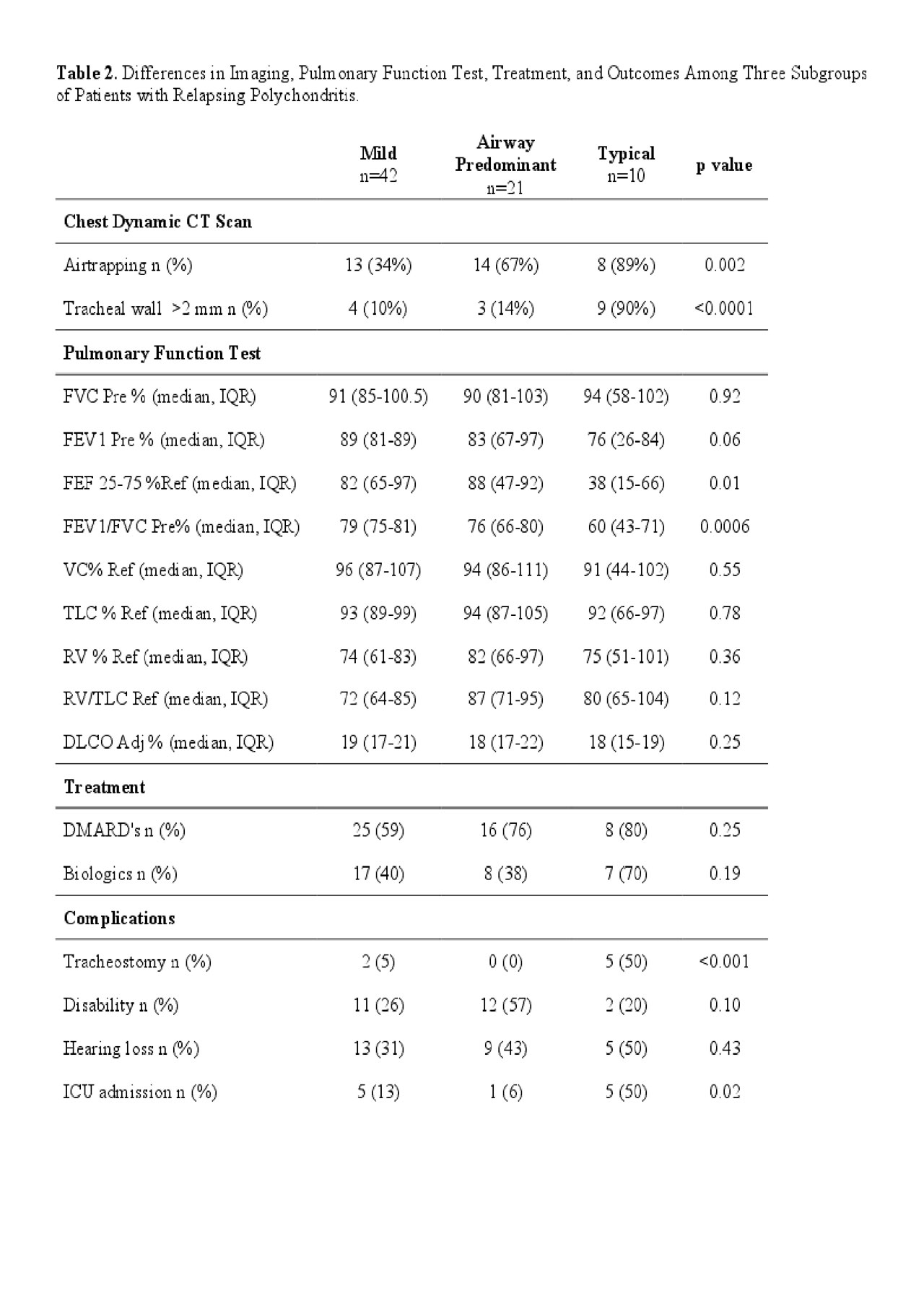
Results: A total of 73 patients were included. Three clusters were identified: Cluster 1 “Typical” (n=10, 14%); Cluster 2 “Airway Predominant” (n=21, 29%); and Cluster 3 “Mild’ (n=42, 57%) (Table 1). Typical RP was characterized by saddle nose deformity (86%), SGS (78%), TM (98%) and ear involvement (98%). Compared to the other clusters, these patients were defined by the shortest time to diagnosis (median = 1 year) and the greatest frequency of weight loss, stridor, air trapping, tracheal wall thickening, decreased FEF 25-75% and FEV1/FVC, ICU admissions, and tracheostomy. Airway Predominant RP was defined by TM (98%) and BM (56%) without saddle nose deformity or SGS and with infrequent ear involvement (41%). Patients in this cluster had the longest delay to diagnosis (median = 10 years) and the greatest percentage of genital ulcers, a previous diagnosis of asthma, and disability. Mild RP was defined by ear involvement (55%) and inflammatory arthritis (41%) without saddle nose deformity, SGS, TM, or BM. These patients had the highest prevalence of skin disease (33%). There were no significant differences in sex, ethnicity, hearing loss, use of DMARDs or biologics between the three clusters. Comparisons between the three clusters are summarized in Table 2.
Conclusion: We identified three phenotypic clusters of patients with RP that differ in time to diagnosis, clinical and radiological characteristics, and complications. Recognizing a broader spectrum of clinical patterns of disease in RP, beyond cartilaginous involvement of the ear and upper airway, may reduce diagnostic delay and facilitate development of targeted management approaches.
To cite this abstract in AMA style:
Ferrada M, Quinn K, Goodspeed W, KIm J, Allen C, Sirajuddin A, Chen M, Gribbons K, Rosenblum J, Rimland C, Katz J, Grayson P. Clinical Phenotypes in Relapsing Polychondritis in a Prospective Cohort [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/clinical-phenotypes-in-relapsing-polychondritis-in-a-prospective-cohort/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-phenotypes-in-relapsing-polychondritis-in-a-prospective-cohort/