Session Information
Date: Tuesday, November 9, 2021
Title: Pediatric Rheumatology – Clinical Poster III: Miscellaneous Rheumatic Disease (1614–1644)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Spread of SARS-COV-2 during the COVID-19 pandemic has raised concerns for patients with rheumatic disease. Rheumatology patients have an increased risk of developing infectious complications due to their underlying disease and chronic use of immunomodulating medications. Reports suggest children with rheumatic disease are not at an increased risk of developing severe symptoms from acute COVID-19; however, there are growing concerns that SARS-COV-2 may trigger their underlying disease, causing exacerbation or new diagnosis of diseases. We report clinical manifestations of SARS-COV-2 and its impact on underlying rheumatic disease activity on pediatric rheumatology patients at our tertiary care center.
Methods: Retrospective chart review of the Children’s Hospital Los Angeles rheumatology clinic population from March 2020 to May 2021 identified pediatric rheumatology patients with reported positive SARS-COV-2 qualitative PCR test and/or positive SARS-COV-2 antibody test. Data including demographics, rheumatic disease diagnosis, medications, co-morbidities, acute symptoms of COVID-19, and rheumatic disease complications were collected. Acute COVID-19 manifestations and rheumatic disease complications (and/or exacerbations) were categorized into numeric scale of 0-3 (COVID-19 manifestations: 0 = No symptoms, 1 = Mild symptoms not requiring hospitalization, 2 = Respiratory distress requiring floor admission, 3 = Respiratory failure requiring intensive care unit (ICU) admission; Rheumatic disease complications: 0 = No flare, 1 = Flare with no escalation of treatment, 2 = Flare requiring escalation of treatment, 3 = Flare requiring hospitalization).
Results: A population of 82 patients of ages 0 to 21 were identified via chart review. Their demographics, diagnosis, medications are included in Table 1. The majority of patients were female (76%) and between ages of 16 to 21 (51%). Most had diagnosis of juvenile idiopathic arthritis (38%) and were taking methotrexate (22%). There were 14 patients with identified co-morbidities, and the most common co-morbidity was obesity (78%). Acute COVID-19 severity scores are demonstrated in Table 2. Most patients scored 1 (55%), followed by 0 (28%). Rheumatic disease complications scores are demonstrated in Table 3. Most patients scored 0 (77%), followed by 3 (13%).
Conclusion: Our findings were consistent with previous reports that many pediatric patients with rheumatic disease experience mild or no symptoms of acute COVID-19. Most patients did not have complications or exacerbations of their underlying disease after contracting SARS-COV-2, although there were cases that required hospitalized care, including those who presented with new-onset rheumatic disease. Autoimmune diseases are often triggered by viral infections, and it may be important for pediatric rheumatologists to pay closer attention to disease activity of patients who contracted SARS-COV-2.
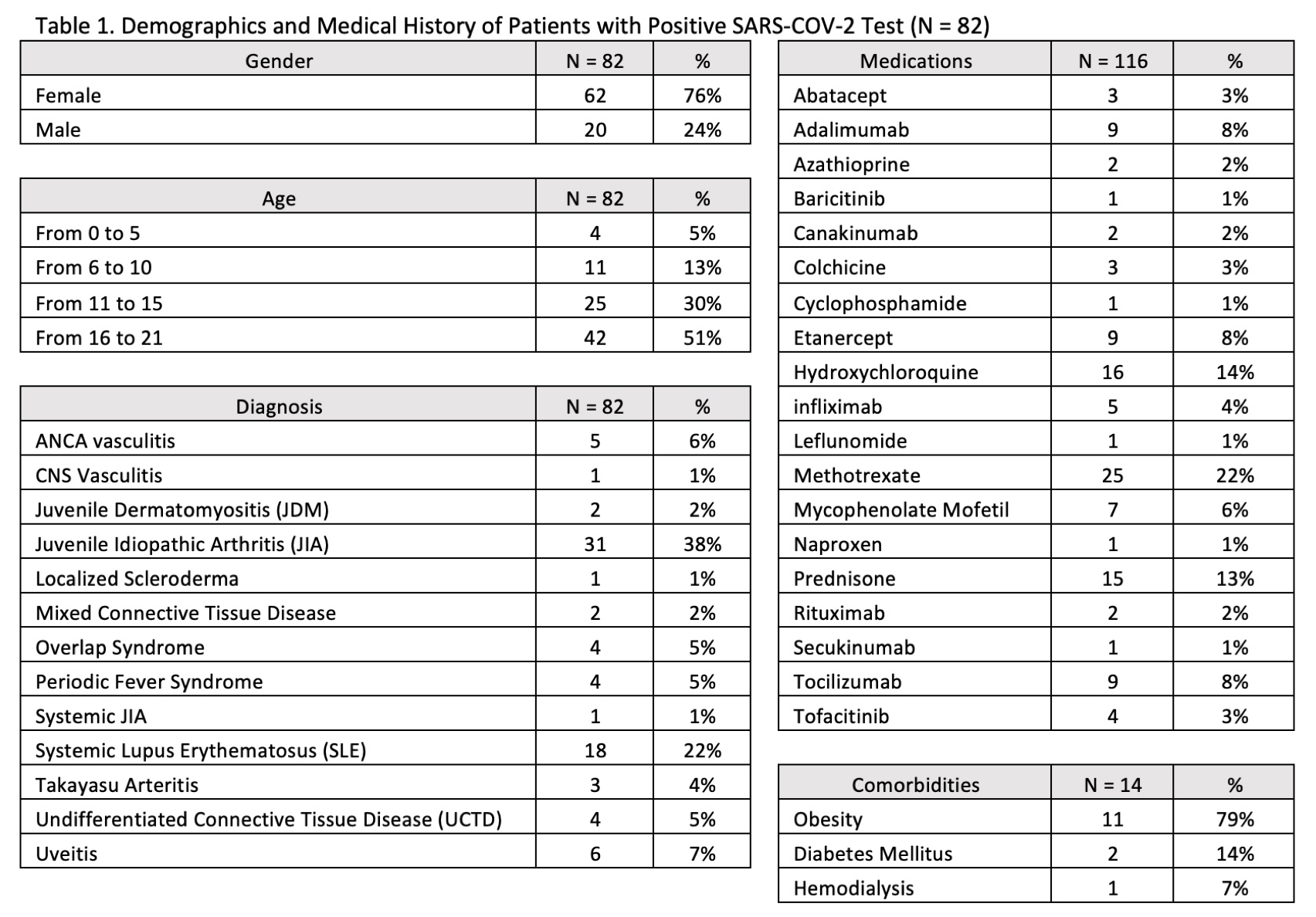 Table 1. Demographics and Medical History of Patients with Positive SARS-COV_2 Test (N = 82)
Table 1. Demographics and Medical History of Patients with Positive SARS-COV_2 Test (N = 82)
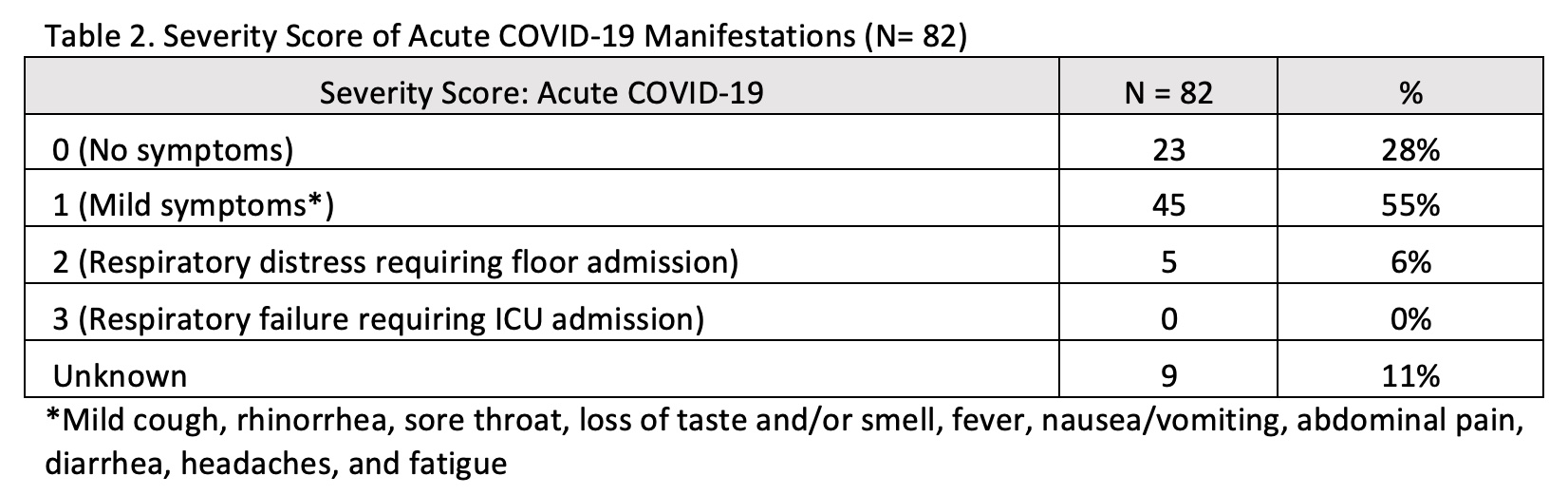 Table 2. Severity Score of Acute COVID_19 Manifestations (Nf 82)
Table 2. Severity Score of Acute COVID_19 Manifestations (Nf 82)
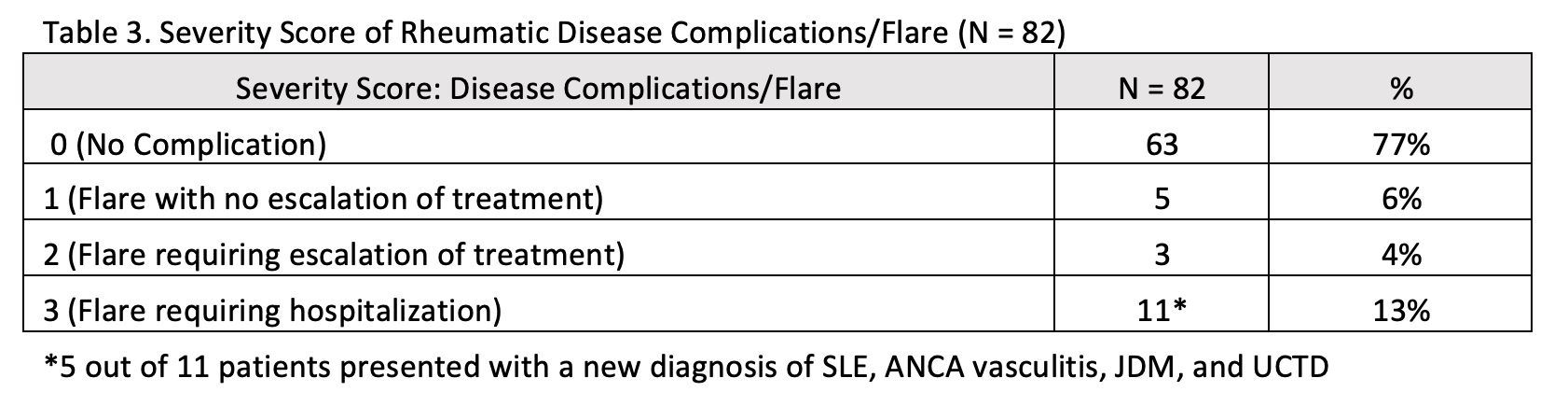 Table 3. Severity Score of Rheumatic Disease Complications/Flare (N = 82)
Table 3. Severity Score of Rheumatic Disease Complications/Flare (N = 82)
To cite this abstract in AMA style:
Yi B, Mohandas S, Cidon M. Clinical Manifestations of COVID-19 and Its Impact on Pediatric Patients with Rheumatic Disease [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/clinical-manifestations-of-covid-19-and-its-impact-on-pediatric-patients-with-rheumatic-disease/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-manifestations-of-covid-19-and-its-impact-on-pediatric-patients-with-rheumatic-disease/
