Session Information
Date: Monday, November 13, 2023
Title: (1442–1487) SLE – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: The impact of COVID-19 in patients with systemic lupus erythematosus (SLE) has been a subject of great concern. Antiviral therapy has emerged as a key approach in the treatment of COVID-19 in the general population, but their efficacy in SLE patients in terms of reducing the risk of hospitalizations, lupus flares, and death remains unclear. Thus, we sought to compare the clinical manifestations and outcomes in SLE patients with COVID-19 that received antiviral therapy to those who did not.
Methods: A cohort of adults (≥21 years) with SLE (per the revised 1997 American College of Rheumatology classification criteria) from a single center in Puerto Rico who had COVID-19 during the Omicron period (December 2021 to December 2022) were studied. SARS CoV-2 infection was confirmed by polymerase chain reaction or antigen tests. Antiviral therapy (nirmatrelvir/ritonavir or molnupiravir) was prescribed to those who presented with mild-to-moderate infection. Demographic parameters, cumulative SLE manifestations, disease activity, damage accrual, lupus treatments, comorbidities, COVID-19 symptoms, emergency room (ER) visits, hospitalizations, SLE flares, and mortality were compared between patients that received antiviral therapy and those who did not using bivariate and multivariate analyses adjusted for age.
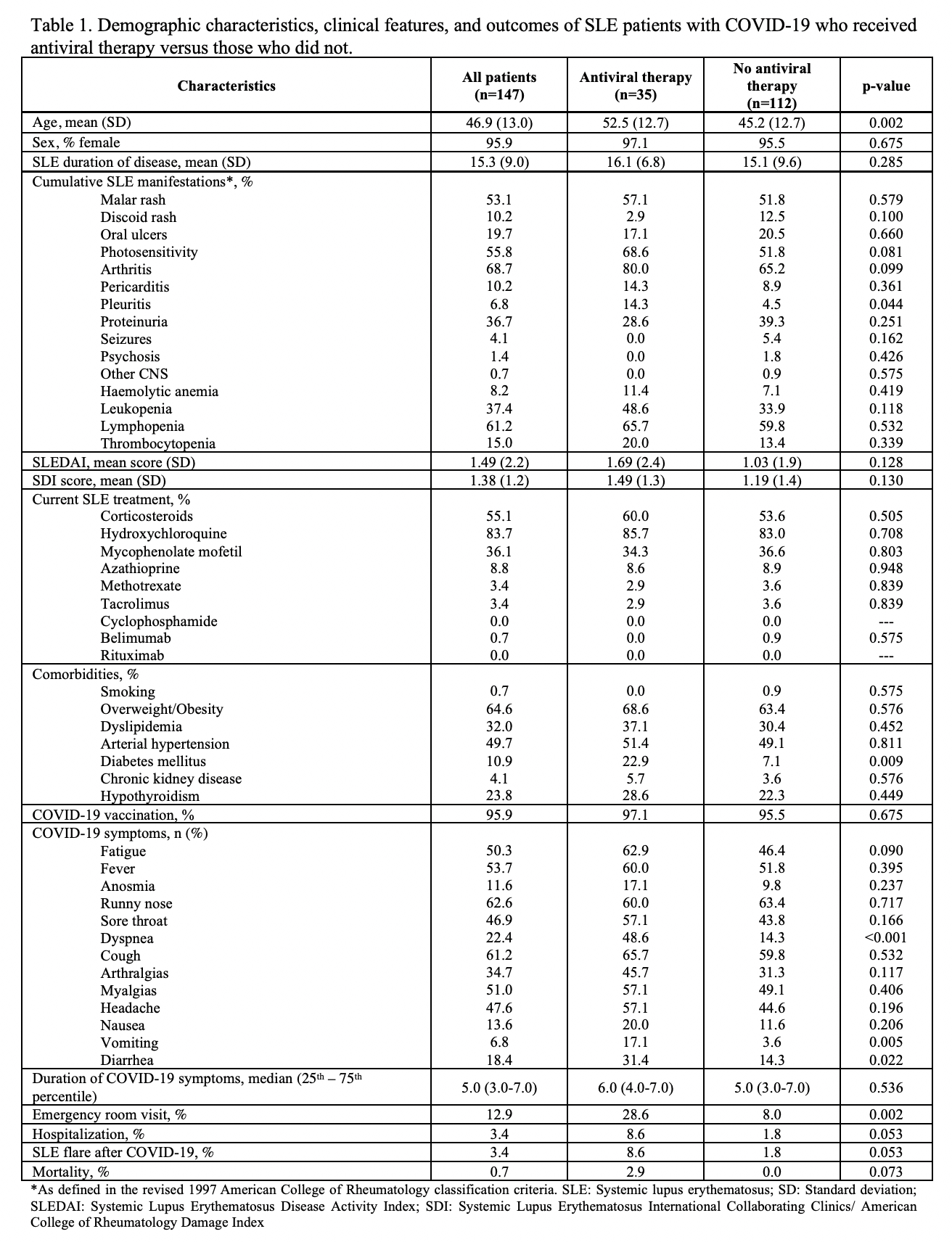
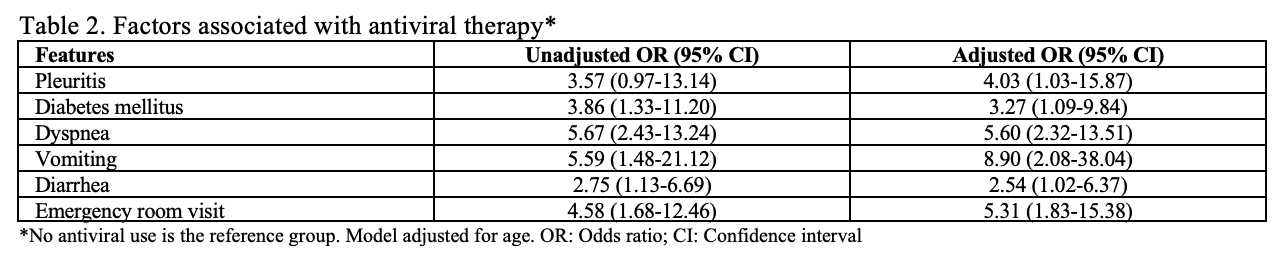
Results: Out of 347 SLE patients, 147 (42.4%) had COVID-19 during the Omicron wave. Among these patients, 35 (23.8%) received antiviral therapy as they presented with mild-to-moderate symptoms. The rest of the cohort had mild symptoms. Older age, pleuritis, diabetes mellitus, some COVID-19 symptoms (dyspnea, vomiting, and diarrhea), and ER visits were significantly more common in patients that received antiviral therapy compared to those who did not (Table 1). All these variables retained significance in the multivariate analysis (Table 2). No significant differences were observed for sex, disease duration, disease activity, disease damage, SLE treatments, hospitalizations, SLE flares, and mortality.
Conclusion: In this cohort of Puerto Ricans with SLE who had COVID-19 during the Omicron period, patients who required antiviral therapy were older and more likely to have pleuritis, diabetes mellitus, and more COVID-19 symptoms than those who did not receive antiviral treatment. Despite having these clinical manifestations and risk factors for severe outcomes, those who were treated with antiviral drugs had a favorable outcome in terms of hospitalizations, SLE flares, and mortality.
To cite this abstract in AMA style:
Serrano-Arroyo L, Ríos-Rivera R, González-Meléndez A, Vilá L. Clinical Manifestations and Outcomes in Systemic Lupus Erythematosus Patients Who Received Antiviral Therapy During the COVID-19 Omicron Variant Wave: Results from a Single Center Cohort of Puerto Rico [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/clinical-manifestations-and-outcomes-in-systemic-lupus-erythematosus-patients-who-received-antiviral-therapy-during-the-covid-19-omicron-variant-wave-results-from-a-single-center-cohort-of-puerto-ric/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-manifestations-and-outcomes-in-systemic-lupus-erythematosus-patients-who-received-antiviral-therapy-during-the-covid-19-omicron-variant-wave-results-from-a-single-center-cohort-of-puerto-ric/