Session Information
Session Type: Poster Session A
Session Time: 6:00PM-7:00PM
Background/Purpose: Takayasu arteritis (TA) is a rare granulomatous vasculitis that affects large vessels, including the aorta, its major branches, and the pulmonary artery. Data on the presentation and clinical course of pediatric TA are limited.
Methods: With an institutional review board approval, a retrospective cohort study of children who were diagnosed with TA at Texas Children’s Hospital between 2005 and 2022 was performed. Data were abstracted from the electronic medical record. Patient demographics, presenting symptoms and signs, imaging findings, and management data were evaluated using standard descriptive statistics.
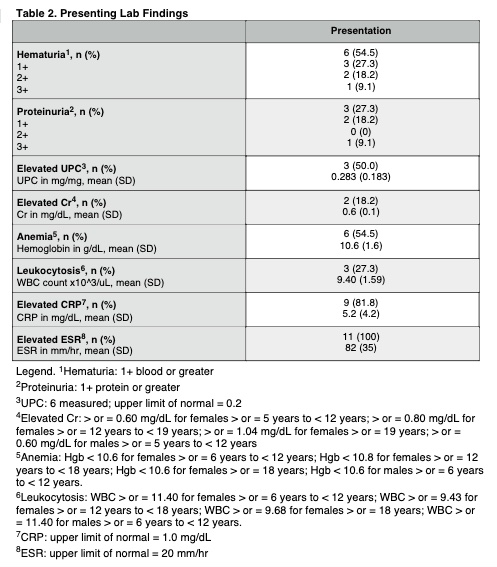
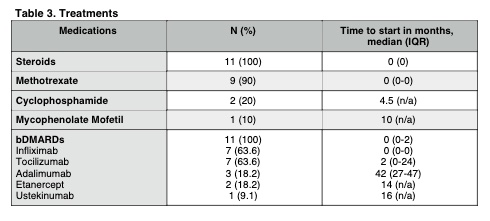
Results: Eleven patients were included. All but one were female (90.9%), with a mean age at diagnosis of 13.5 years (range 9-17). Most were Hispanic or Latino (63.6%). Diagnosis was made a median of 4 months following symptom onset (IQR 1-15), and the mean follow up period was 45.7 months (range 7-112). The most common symptoms on presentation were constitutional, with all patients having at least one of fatigue (90.9%), weight loss (81.8%), or fever (36.4%). Only one patient had claudication. Hypertension (54.5%) was the most common exam finding. All patients had an elevated ESR (mean 82 mm/hr, range 25-146), and all but two had an elevated CRP (mean 5.2, range 0.2-13.6). All patients had imaging evidence of aortic involvement, including the abdominal (72.7%), ascending thoracic (63.6%), and descending thoracic (54.5%) segments. All patients were started on systemic corticosteroids at the time of diagnosis. Initial steroid sparing immunomodulatory agents included a combination of Methotrexate and Infliximab in most patients (54.5%). Two were started on Tocilizumab alone, two were started on Methotrexate alone (both diagnosed on or prior to 2010), and one was not started on therapy beyond steroids at the initial encounter due to diagnostic uncertainty. All patients were on a biologic DMARD (bDMARD) at some point in their disease course, with a median time to start of 0 months (IQR 0-2). Reasons for addition or change of therapy included poor disease control or flare, inability to wean steroids, new disease manifestations, infusion reactions, side effects, and ease of administration. Four patients (36.4%) required surgical management. At the most recent follow-up visit, only four patients remained on steroids. One patient was off all medications completely and remained in clinical remission. All but three patients were asymptomatic, and there was a statistically significant decrease in ESR (p=0.01) and CRP (p=0.02) from the initial to the final visit.
Conclusion: Like prior studies, patients in our cohort presented predominantly with constitutional symptoms, hypertension, and elevated inflammatory markers. bDMARDs were introduced earlier in disease course than in previously reported cohorts. Outcomes were generally favorable, and most patients were symptom-free off steroids at the most recent follow-up. However, patients were not often able to wean off all medications.
To cite this abstract in AMA style:
Altaffer A, Orjuela A, De Guzman M. Clinical Manifestations and Management of Takayasu Arteritis: A Single Center Pediatric Cohort [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/clinical-manifestations-and-management-of-takayasu-arteritis-a-single-center-pediatric-cohort/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-manifestations-and-management-of-takayasu-arteritis-a-single-center-pediatric-cohort/